Sunday Poster Session
Category: Liver
P1147 - Use of Sodium-Glucose Transport Protein 2 Inhibitors and Dipeptidyl Peptidase 4 Inhibitors in Patients with MASLD in a Real-World Setting is Associated with Lower All-Cause Mortality
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- SH
Sophia Hurr, BSPH
University of North Carolina at Chapel Hill School of Medicine
Chapel Hill, NC
Presenting Author(s)
Sophia Hurr, BSPH1, Breda Munoz, PhD2, Andrea Rossi. Mospan, PhD, RAC2, Michael Roden, MD3, Kenneth Cusi, MD4, Alfred S. Barritt, MD, MSCR5
1University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 2Target RWE, Durham, NC; 3Heinrich Heine University, Dusseldorf, Nordrhein-Westfalen, Germany; 4University of Florida College of Medicine, Gainesville, FL; 5UNC, Chapel Hill, NC
Introduction: While there has been an increasing focus on using glucagon-like peptide 1 receptor agonists for the treatment of metabolic dysfunction associated steatotic liver disease (MASLD), other glucose lowering drugs like sodium-glucose transport protein 2 inhibitors (SGLT2) and dipeptidyl peptidase 4 inhibitors (DPP4) have been less studied in liver disease. This analysis aims to describe patient characteristics and outcomes in patients with MASLD who use SGLT2 or DPP4 medications.
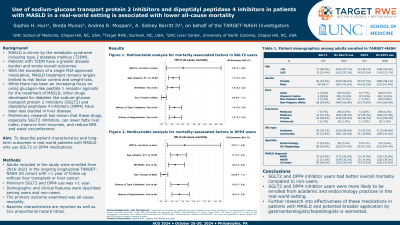
Methods: Adults included in the study were enrolled from 2016-2023 in the TARGET-NASH US cohort with >1 year of follow up without liver transplant or liver cancer. Minimum SGLT2 and DPP4 use was >1 year. Demographic and clinical features were described among users and non-users. The primary outcome was all-cause mortality. Baseline characteristics are reported as well as Cox proportional hazard ratios.
Results: There were 3712 adult patients from the TARGET-NASH US cohort who met inclusion criteria. Overall, 105 (3%) used SGLT2 medications and 104 (3%) used DPP4 medications. There were no differences in age, sex, insurance type among SGLT2 users and non-users. Compared to non-users, SGLT2 users were more likely Caucasian (84% vs 67%, p=0.006), had higher BMI (34 vs 32 kg/m2 p=0.007), seen at an academic site (78% vs 58% p< 0.001), enrolled by endocrinologists (16% vs 2% p< 0.001), and had higher prevalence of cardiovascular disease, hypertension, dyslipidemia, and diabetes (all p< 0.05). Among SGLT2 users, 24 (23%) had MASL, 12 (11%) MASH and 69 (66%) cirrhosis. Compared to non-users, DPP4 users were older (65 vs 58 years, p< 0.001) Caucasian (80% vs 67%, p=0.04), insured by Medicare (45% vs 28%, p=0.004), seen at an academic site (70% vs 59% p=0.018), enrolled by endocrinologists (9% vs 3% p=0.007), and had higher prevalence of cardiovascular disease, hypertension, dyslipidemia, and diabetes (all p< 0.05). Among DPP4 users, 15 (14%) had MASL, 15 (14%) MASH and 74 (72%) cirrhosis. The HR for overall mortality in SGLT2 non-users vs users was 2.57 (95% CI 1.13, 5.82). The HR for overall mortality in DPP4 non-users vs users was 2.22 (95% CI 1.08, 4.53).
Discussion: SGLT2 and DPP4 users were more likely to be enrolled from academic and endocrinology practices and had better overall survival than non-users in this real-world setting. Further research into effectiveness of these medications in patients with MASLD and broader application by gastroenterologists/hepatologists is warranted.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sophia Hurr, BSPH1, Breda Munoz, PhD2, Andrea Rossi. Mospan, PhD, RAC2, Michael Roden, MD3, Kenneth Cusi, MD4, Alfred S. Barritt, MD, MSCR5. P1147 - Use of Sodium-Glucose Transport Protein 2 Inhibitors and Dipeptidyl Peptidase 4 Inhibitors in Patients with MASLD in a Real-World Setting is Associated with Lower All-Cause Mortality, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 2Target RWE, Durham, NC; 3Heinrich Heine University, Dusseldorf, Nordrhein-Westfalen, Germany; 4University of Florida College of Medicine, Gainesville, FL; 5UNC, Chapel Hill, NC
Introduction: While there has been an increasing focus on using glucagon-like peptide 1 receptor agonists for the treatment of metabolic dysfunction associated steatotic liver disease (MASLD), other glucose lowering drugs like sodium-glucose transport protein 2 inhibitors (SGLT2) and dipeptidyl peptidase 4 inhibitors (DPP4) have been less studied in liver disease. This analysis aims to describe patient characteristics and outcomes in patients with MASLD who use SGLT2 or DPP4 medications.
Methods: Adults included in the study were enrolled from 2016-2023 in the TARGET-NASH US cohort with >1 year of follow up without liver transplant or liver cancer. Minimum SGLT2 and DPP4 use was >1 year. Demographic and clinical features were described among users and non-users. The primary outcome was all-cause mortality. Baseline characteristics are reported as well as Cox proportional hazard ratios.
Results: There were 3712 adult patients from the TARGET-NASH US cohort who met inclusion criteria. Overall, 105 (3%) used SGLT2 medications and 104 (3%) used DPP4 medications. There were no differences in age, sex, insurance type among SGLT2 users and non-users. Compared to non-users, SGLT2 users were more likely Caucasian (84% vs 67%, p=0.006), had higher BMI (34 vs 32 kg/m2 p=0.007), seen at an academic site (78% vs 58% p< 0.001), enrolled by endocrinologists (16% vs 2% p< 0.001), and had higher prevalence of cardiovascular disease, hypertension, dyslipidemia, and diabetes (all p< 0.05). Among SGLT2 users, 24 (23%) had MASL, 12 (11%) MASH and 69 (66%) cirrhosis. Compared to non-users, DPP4 users were older (65 vs 58 years, p< 0.001) Caucasian (80% vs 67%, p=0.04), insured by Medicare (45% vs 28%, p=0.004), seen at an academic site (70% vs 59% p=0.018), enrolled by endocrinologists (9% vs 3% p=0.007), and had higher prevalence of cardiovascular disease, hypertension, dyslipidemia, and diabetes (all p< 0.05). Among DPP4 users, 15 (14%) had MASL, 15 (14%) MASH and 74 (72%) cirrhosis. The HR for overall mortality in SGLT2 non-users vs users was 2.57 (95% CI 1.13, 5.82). The HR for overall mortality in DPP4 non-users vs users was 2.22 (95% CI 1.08, 4.53).
Discussion: SGLT2 and DPP4 users were more likely to be enrolled from academic and endocrinology practices and had better overall survival than non-users in this real-world setting. Further research into effectiveness of these medications in patients with MASLD and broader application by gastroenterologists/hepatologists is warranted.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sophia Hurr indicated no relevant financial relationships.
Breda Munoz indicated no relevant financial relationships.
Andrea Mospan: Target RWE – Employee.
Michael Roden: Target RWE – Consultant.
Kenneth Cusi: Target RWE – Consultant.
Alfred Barritt: Boehringer Ingelheim – Consultant. Merck (Any division) – Consultant. Target RWE – Consultant.
Sophia Hurr, BSPH1, Breda Munoz, PhD2, Andrea Rossi. Mospan, PhD, RAC2, Michael Roden, MD3, Kenneth Cusi, MD4, Alfred S. Barritt, MD, MSCR5. P1147 - Use of Sodium-Glucose Transport Protein 2 Inhibitors and Dipeptidyl Peptidase 4 Inhibitors in Patients with MASLD in a Real-World Setting is Associated with Lower All-Cause Mortality, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
