Sunday Poster Session
Category: Interventional Endoscopy
P1066 - EUS-Guided Gastroenterostomy for Benign Gastric Outlet Obstruction: A Systematic Review and Meta-Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Nicol Tugarinov, BS
University of Maryland School of Medicine
Baltimore, MD
Presenting Author(s)
Andrew Canakis, DO1, Nicol Tugarinov, BS2, Jay Bapaye, MD3, Benjamin Twery, MD2, Justin Canakis, DO4, Abdulhameed Al-Sabban, MD5, Shayan Irani, MD6
1University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 2University of Maryland School of Medicine, Baltimore, MD; 3Virginia Tech Carilion School of Medicine, Roanoke, VA; 4Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 5University of Maryland Medical Center, Baltimore, MD; 6Virginia Mason Franciscan Health, Seattle, WA
Introduction: Gastric outlet obstruction (GOO) is a clinical manifestation of obstruction at the antropyloric region or proximal small bowel that can lead to progressive symptoms of nausea, vomiting, weight loss, volume depletion and malnutrition. The degree of mechanical blockage correlates with symptom severity. The goal of endoscopic management is to relieve the obstruction so individuals can resume per oral intake and thus improve quality of life metrics.
Most studies have involved malignant causes of GOO; yet only a handful of studies have explored outcomes related to benign etiologies. Management options for benign GOO includes endoscopic balloon dilation, fully covered self-expanding metal stent placement, and lumen apposing metal stent (LAMS) placement across the stricture. Recently, endoscopic ultrasound-guided gastroenterostomy (EUS-GE) has emerged as a novel method to bypass the obstruction with a LAMS. In this systematic review and meta-analysis, we aim to explore the technical success and clinical outcomes of EUS-GE for benign GOO.
Methods: Multiple databases were searched for studies looking at EUS-GE for benign GOO from inception until May 2024. The primary outcome was technical and clinical success. Secondary outcomes included rate of reintervention and adverse events (AE).
Results: Nine studies met inclusion criteria with 150 patients treated with EUS-GE for benign GOO (Table 1). The most common etiologies were from chronic (n=48) and acute (n=41) pancreatitis. The direct technique was utilized in most cases (n=80), and the mean procedure time was 51.2 minutes.
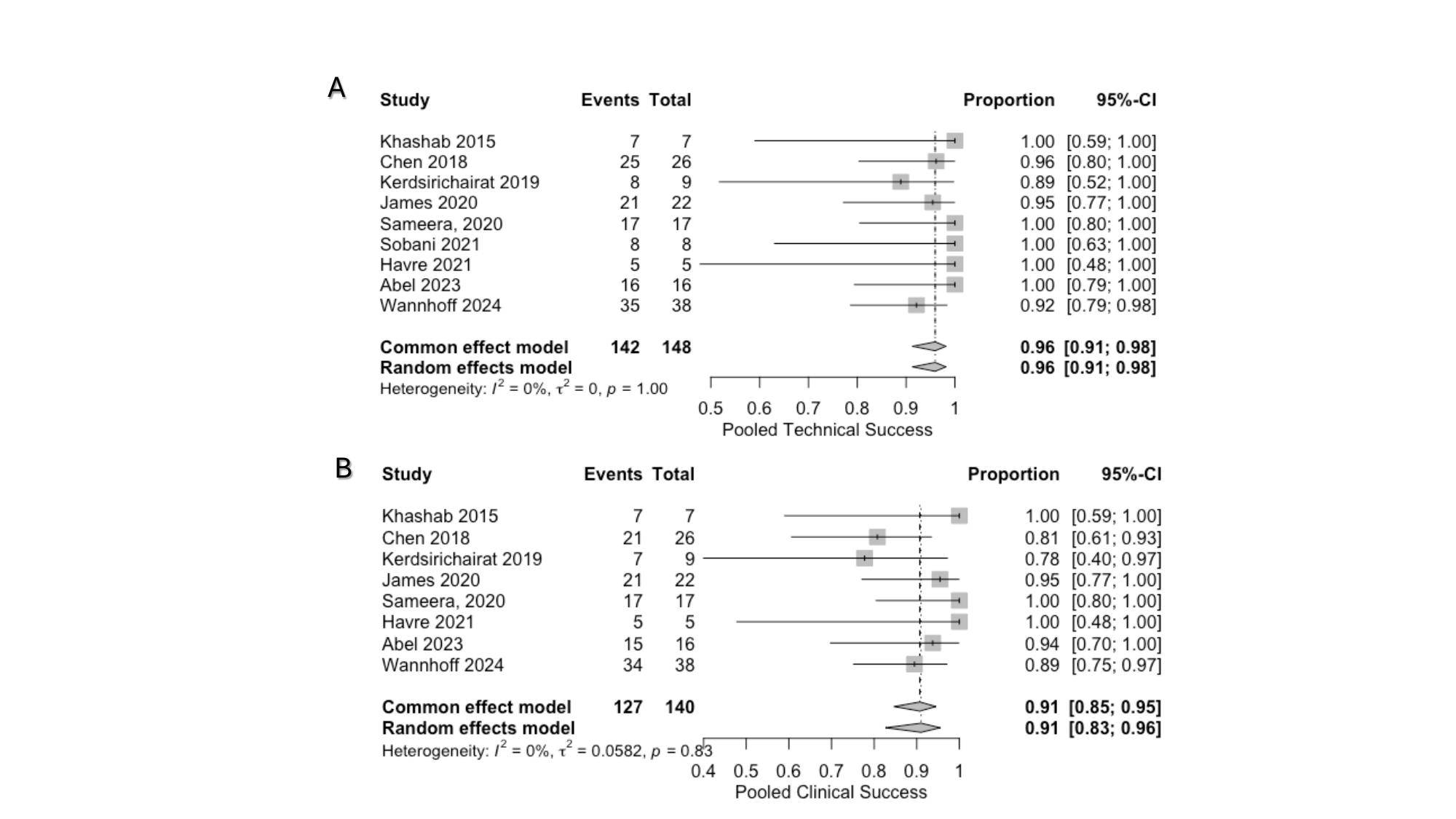
The pooled technical success rate was 95.5% (95% confidence interval (CI), 91.27-98.17; I2 = 0%) and clinical success rate was 91% (95% CI, 82.66-95.5; I2 = 0%) (Figure 1). The rates of reintervention and AE were 9.27% (95% CI, 3.92-20.39; I2 = 42%) and 7.63% (95% CI, 3.78-14.8; I2 = 0%), respectively.
Discussion: The results of this meta-analysis demonstrate the efficacy and relative safety profile of EUS-GE for benign GOO. Further comparative studies are needed to determine the optimal treatment strategy in this select patient population based on the underlying etiology and treatment modality (i.e. enteral stenting).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Andrew Canakis, DO1, Nicol Tugarinov, BS2, Jay Bapaye, MD3, Benjamin Twery, MD2, Justin Canakis, DO4, Abdulhameed Al-Sabban, MD5, Shayan Irani, MD6. P1066 - EUS-Guided Gastroenterostomy for Benign Gastric Outlet Obstruction: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 2University of Maryland School of Medicine, Baltimore, MD; 3Virginia Tech Carilion School of Medicine, Roanoke, VA; 4Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 5University of Maryland Medical Center, Baltimore, MD; 6Virginia Mason Franciscan Health, Seattle, WA
Introduction: Gastric outlet obstruction (GOO) is a clinical manifestation of obstruction at the antropyloric region or proximal small bowel that can lead to progressive symptoms of nausea, vomiting, weight loss, volume depletion and malnutrition. The degree of mechanical blockage correlates with symptom severity. The goal of endoscopic management is to relieve the obstruction so individuals can resume per oral intake and thus improve quality of life metrics.
Most studies have involved malignant causes of GOO; yet only a handful of studies have explored outcomes related to benign etiologies. Management options for benign GOO includes endoscopic balloon dilation, fully covered self-expanding metal stent placement, and lumen apposing metal stent (LAMS) placement across the stricture. Recently, endoscopic ultrasound-guided gastroenterostomy (EUS-GE) has emerged as a novel method to bypass the obstruction with a LAMS. In this systematic review and meta-analysis, we aim to explore the technical success and clinical outcomes of EUS-GE for benign GOO.
Methods: Multiple databases were searched for studies looking at EUS-GE for benign GOO from inception until May 2024. The primary outcome was technical and clinical success. Secondary outcomes included rate of reintervention and adverse events (AE).
Results: Nine studies met inclusion criteria with 150 patients treated with EUS-GE for benign GOO (Table 1). The most common etiologies were from chronic (n=48) and acute (n=41) pancreatitis. The direct technique was utilized in most cases (n=80), and the mean procedure time was 51.2 minutes.
The pooled technical success rate was 95.5% (95% confidence interval (CI), 91.27-98.17; I2 = 0%) and clinical success rate was 91% (95% CI, 82.66-95.5; I2 = 0%) (Figure 1). The rates of reintervention and AE were 9.27% (95% CI, 3.92-20.39; I2 = 42%) and 7.63% (95% CI, 3.78-14.8; I2 = 0%), respectively.
Discussion: The results of this meta-analysis demonstrate the efficacy and relative safety profile of EUS-GE for benign GOO. Further comparative studies are needed to determine the optimal treatment strategy in this select patient population based on the underlying etiology and treatment modality (i.e. enteral stenting).
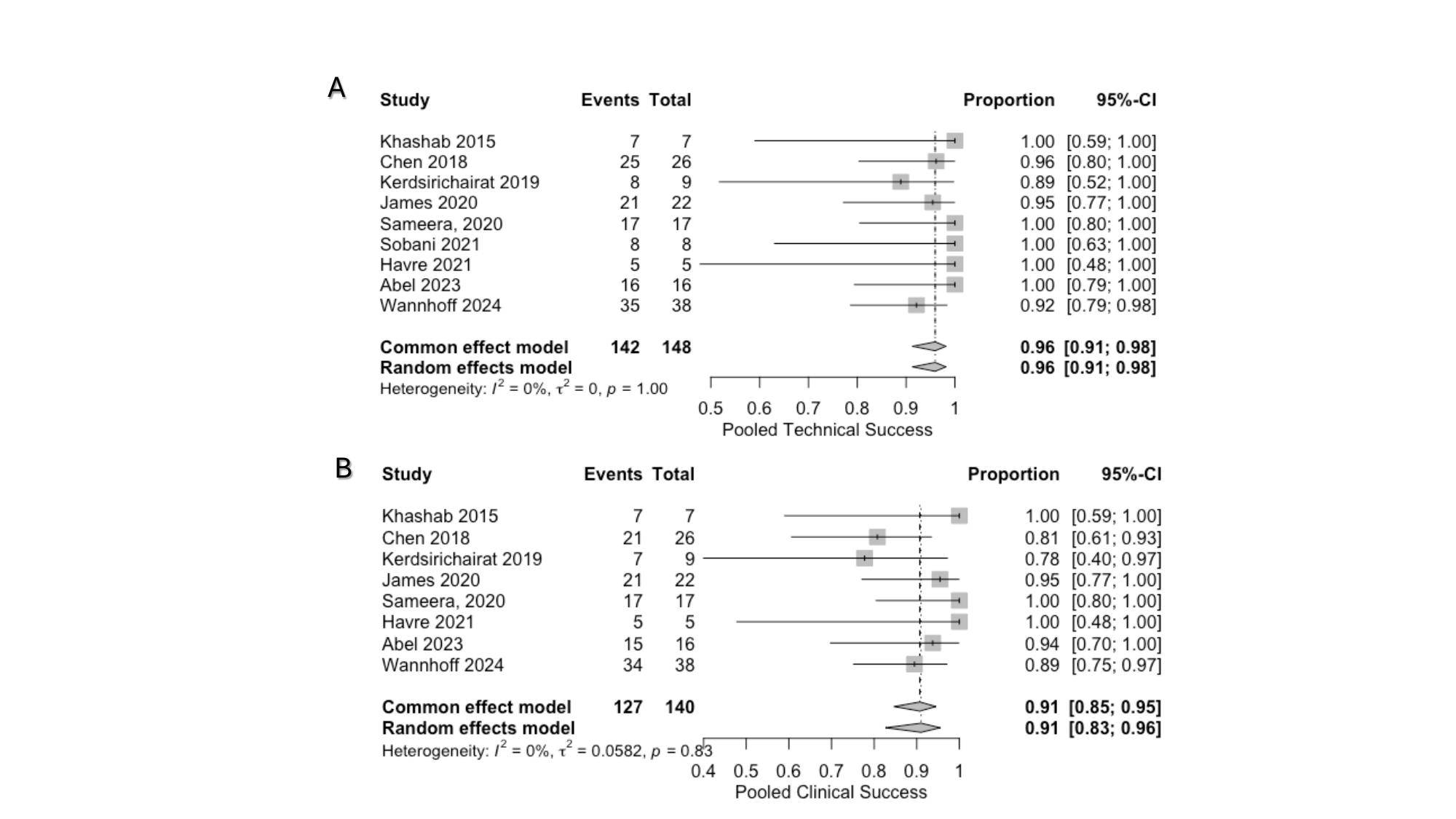
Figure: Forest plot of technical (A) and clinical success (B) rates
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Andrew Canakis indicated no relevant financial relationships.
Nicol Tugarinov indicated no relevant financial relationships.
Jay Bapaye indicated no relevant financial relationships.
Benjamin Twery indicated no relevant financial relationships.
Justin Canakis indicated no relevant financial relationships.
Abdulhameed Al-Sabban indicated no relevant financial relationships.
Shayan Irani: Boston Scientific – Consultant. Conmed – Consultant. Gore – Consultant.
Andrew Canakis, DO1, Nicol Tugarinov, BS2, Jay Bapaye, MD3, Benjamin Twery, MD2, Justin Canakis, DO4, Abdulhameed Al-Sabban, MD5, Shayan Irani, MD6. P1066 - EUS-Guided Gastroenterostomy for Benign Gastric Outlet Obstruction: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
