Sunday Poster Session
Category: Interventional Endoscopy
P1070 - Therapeutic Endoscopic Retrograde Cholangiopancreatography in Patients With Cirrhosis: A 5-year Nationwide Analysis of Sociodemographic Characteristics and Inpatient Outcomes
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Medha Rajamanuri, MBBS
Southern Illinois University
springfield, IL
Presenting Author(s)
Medha Rajamanuri, MBBS1, Sai Shanmukha Sreeram Pannala, MD2, Hima Varsha. Voruganti, MBBS, MD3, Hafiz Sharjeel Arshad, MD1
1Southern Illinois University, Springfield, IL; 2Staten Island University Hospital, Northwell Health, Staten Island, NY; 3North Alabama Medical Center, Florence, AL
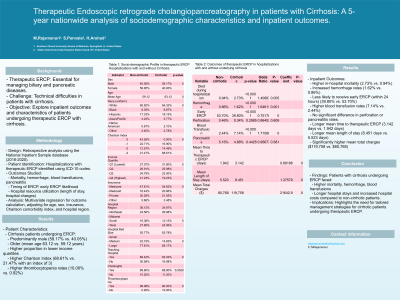
Introduction: Therapeutic ERCP stands as a vital procedure in managing biliary and pancreatic diseases. Nevertheless, it poses a technical challenge especially in patients with cirrhosis. We aim to explore the impact of underlying cirrhosis on inpatient outcomes, timing of ERCP and study the baseline characteristics of patients undergoing therapeutic ERCP in the hospital in recent years.
Methods: We conducted a retrospective analysis using the National Inpatient Sample database from 2016 to 2020. Hospitalizations undergoing therapeutic ERCP were identified using ICD-10 codes, and their socio-demographic characteristics and inpatient outcomes—including mortality, hemorrhage, need for blood transfusions, pancreatitis, likelihood of receiving an early ERCP, and mean time to therapeutic ERCP—were studied. Additionally, their utilization of hospital resources, such as length of stay and hospital charges, was examined. Multivariate regression analysis was employed to calculate the outcomes, adjusting for confounding factors including age, sex, insurance, Charlson comorbidity index, hospital region.
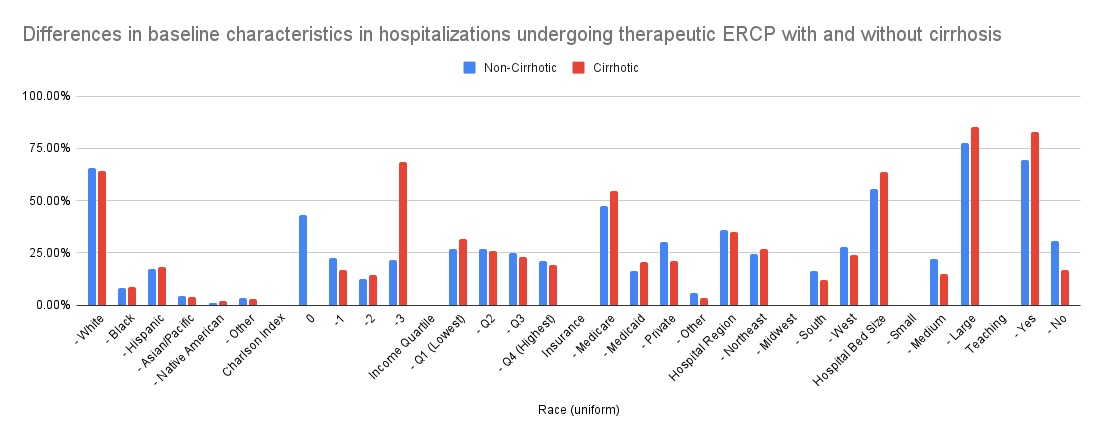
Results: In comparing hospitalizations undergoing therapeutic ERCP with and without cirrhosis, several key differences emerge. Cirrhosis patients were predominantly male (59.17% vs. 40.05%) and older (mean age 63.12 vs. 59.12 years), with a higher proportion in lower income quartiles and a higher Charlson Index (68.61% vs. 21.47% with an index of 3). They also had lower cholangitis (16.98% vs. 30.58%) and higher rates of thrombocytopenia (10.00% vs. 0.92%)
Among the hospitalizations undergoing therapeutic ERCP, those with cirrhosis experienced higher in-hospital mortality (2.73% vs. 0.94%) and hemorrhage (1.62% vs. 0.86%). They were less likely to undergo early ERCP (within 24 hours) (39.80% vs. 53.70%) and more likely to require blood transfusion (7.14% vs. 2.44%).
No significant difference was found in perforation rates or pancreatitis occurrence between the two groups. Cirrhotic hospitalizations had longer mean time to therapeutic ERCP (3.142 days vs. 1.942 days) and longer mean length of stay (8.451 days vs. 5.523 days), with significantly higher mean total charges ($119,758 vs. $80,768).
Discussion:
In summary, patients undergoing ERCP with cirrhosis faced more significant challenges, including higher rates of mortality, hemorrhage, blood transfusion, longer hospital stays, and higher hospital costs compared to those without cirrhosis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Medha Rajamanuri, MBBS1, Sai Shanmukha Sreeram Pannala, MD2, Hima Varsha. Voruganti, MBBS, MD3, Hafiz Sharjeel Arshad, MD1. P1070 - Therapeutic Endoscopic Retrograde Cholangiopancreatography in Patients With Cirrhosis: A 5-year Nationwide Analysis of Sociodemographic Characteristics and Inpatient Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Southern Illinois University, Springfield, IL; 2Staten Island University Hospital, Northwell Health, Staten Island, NY; 3North Alabama Medical Center, Florence, AL
Introduction: Therapeutic ERCP stands as a vital procedure in managing biliary and pancreatic diseases. Nevertheless, it poses a technical challenge especially in patients with cirrhosis. We aim to explore the impact of underlying cirrhosis on inpatient outcomes, timing of ERCP and study the baseline characteristics of patients undergoing therapeutic ERCP in the hospital in recent years.
Methods: We conducted a retrospective analysis using the National Inpatient Sample database from 2016 to 2020. Hospitalizations undergoing therapeutic ERCP were identified using ICD-10 codes, and their socio-demographic characteristics and inpatient outcomes—including mortality, hemorrhage, need for blood transfusions, pancreatitis, likelihood of receiving an early ERCP, and mean time to therapeutic ERCP—were studied. Additionally, their utilization of hospital resources, such as length of stay and hospital charges, was examined. Multivariate regression analysis was employed to calculate the outcomes, adjusting for confounding factors including age, sex, insurance, Charlson comorbidity index, hospital region.
Results: In comparing hospitalizations undergoing therapeutic ERCP with and without cirrhosis, several key differences emerge. Cirrhosis patients were predominantly male (59.17% vs. 40.05%) and older (mean age 63.12 vs. 59.12 years), with a higher proportion in lower income quartiles and a higher Charlson Index (68.61% vs. 21.47% with an index of 3). They also had lower cholangitis (16.98% vs. 30.58%) and higher rates of thrombocytopenia (10.00% vs. 0.92%)
Among the hospitalizations undergoing therapeutic ERCP, those with cirrhosis experienced higher in-hospital mortality (2.73% vs. 0.94%) and hemorrhage (1.62% vs. 0.86%). They were less likely to undergo early ERCP (within 24 hours) (39.80% vs. 53.70%) and more likely to require blood transfusion (7.14% vs. 2.44%).
No significant difference was found in perforation rates or pancreatitis occurrence between the two groups. Cirrhotic hospitalizations had longer mean time to therapeutic ERCP (3.142 days vs. 1.942 days) and longer mean length of stay (8.451 days vs. 5.523 days), with significantly higher mean total charges ($119,758 vs. $80,768).
Discussion:
In summary, patients undergoing ERCP with cirrhosis faced more significant challenges, including higher rates of mortality, hemorrhage, blood transfusion, longer hospital stays, and higher hospital costs compared to those without cirrhosis.
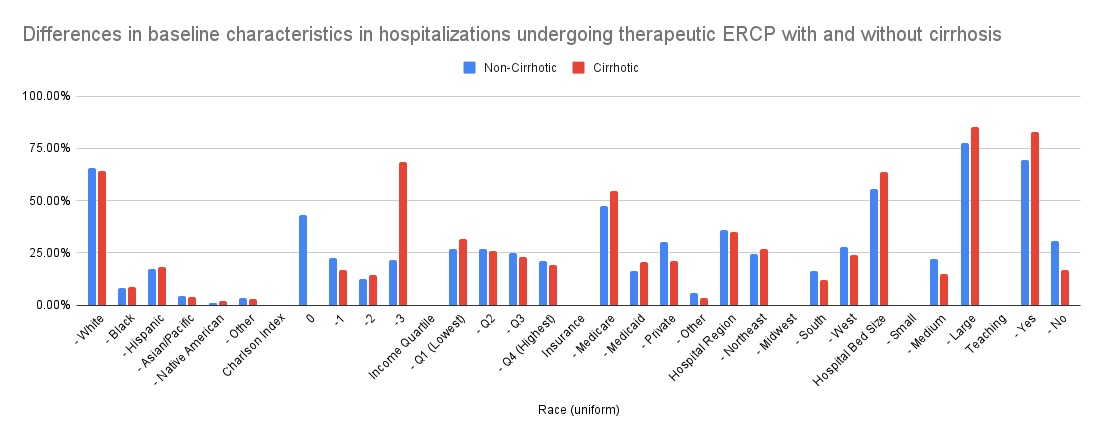
Figure: Socio-demographic Profile in therapeutic ERCP Hospitalizations with and without Cirrhosis
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Medha Rajamanuri indicated no relevant financial relationships.
Sai Shanmukha Sreeram Pannala indicated no relevant financial relationships.
Hima Voruganti indicated no relevant financial relationships.
Hafiz Sharjeel Arshad indicated no relevant financial relationships.
Medha Rajamanuri, MBBS1, Sai Shanmukha Sreeram Pannala, MD2, Hima Varsha. Voruganti, MBBS, MD3, Hafiz Sharjeel Arshad, MD1. P1070 - Therapeutic Endoscopic Retrograde Cholangiopancreatography in Patients With Cirrhosis: A 5-year Nationwide Analysis of Sociodemographic Characteristics and Inpatient Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
