Sunday Poster Session
Category: Interventional Endoscopy
P1078 - Novel Endoscopic Approach of Transluminal Drainage for Deep Pelvic Collections in Acute Necrotizing Pancreatitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Benjamin E. Hoffman, MD
Tufts Medical Center
Boston, MA
Presenting Author(s)
Benjamin E. Hoffman, MD, Jennifer Youn, MD, Manoj Kumar, MD
Tufts Medical Center, Boston, MA
Introduction: Necrotizing pancreatitis is a major complication of acute pancreatitis. Endoscopic step-up approaches are used to drain associated fluid collections. However, collections that extend into the deep pelvis often require percutaneous drainage catheters (PCD). We present a case of necrotizing pancreatitis with deep pelvic collections that were successfully drained via endoscopic transluminal drainage.
Case Description/Methods: A 54-year-old male with remote history of alcohol use presented with acute onset of epigastric pain. Physical exam was notable for abdominal distension. Laboratory results showed white blood cell count 26 K/uL, lipase 588 U/L, and triglycerides of 59 mg/dL. An abdominal ultrasound did not show gallstones. Computed tomography (CT) of abdomen and pelvis showed necrotizing pancreatitis with acute necrotic collections. Serial CT scans showed evolution of the multiloculated collections including confluence and extension to the lesser sac, paracolic gutters, and pelvis. The collection measured 15 x 11 cm prior to intervention.
Using multiple transluminal gateway technique, a lumen apposing metal stent (LAMS) was placed at the proximal stomach wall with establishment of cystgastrostomy. A necrosectomy was performed and a 7F x 10 cm double pigtail stent was deployed through the LAMS. A second LAMS was placed distally and two 7F x 28 cm double pigtail stents were deployed over a guidewire under fluoroscopic guidance into the deeper pelvic collections. These stents were exchanged and upsized on subsequent necrosectomies. Interval abdominal imaging showed a significant decrease in the fluid collection size to 7.5 x 5.7 cm prior to discharge. Serially imaging demonstrated a continued decrease in collection size in the outpatient setting.
Discussion: Current management of acute necrotizing pancreatitis utilizes a step-up approach, relegating open necrosectomy as a last resort. Exclusive endoscopic approach for management is only achieved in 60% of patients. In remaining patients, adjunctive PCD is required. PCD confers risk of development of pancreaticocutaneous or enterocutaneous fistulas. Indwelling catheters are also associated with impaired quality of life for patients. This novel endoscopic approach resulted in marked improvement in deep fluid collections normally reserved for PCD. Future advances in endoscopic techniques may result in a higher proportion of endoscopic exclusivity in the management of fluid collections associated with necrotizing pancreatitis.

Disclosures:
Benjamin E. Hoffman, MD, Jennifer Youn, MD, Manoj Kumar, MD. P1078 - Novel Endoscopic Approach of Transluminal Drainage for Deep Pelvic Collections in Acute Necrotizing Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Tufts Medical Center, Boston, MA
Introduction: Necrotizing pancreatitis is a major complication of acute pancreatitis. Endoscopic step-up approaches are used to drain associated fluid collections. However, collections that extend into the deep pelvis often require percutaneous drainage catheters (PCD). We present a case of necrotizing pancreatitis with deep pelvic collections that were successfully drained via endoscopic transluminal drainage.
Case Description/Methods: A 54-year-old male with remote history of alcohol use presented with acute onset of epigastric pain. Physical exam was notable for abdominal distension. Laboratory results showed white blood cell count 26 K/uL, lipase 588 U/L, and triglycerides of 59 mg/dL. An abdominal ultrasound did not show gallstones. Computed tomography (CT) of abdomen and pelvis showed necrotizing pancreatitis with acute necrotic collections. Serial CT scans showed evolution of the multiloculated collections including confluence and extension to the lesser sac, paracolic gutters, and pelvis. The collection measured 15 x 11 cm prior to intervention.
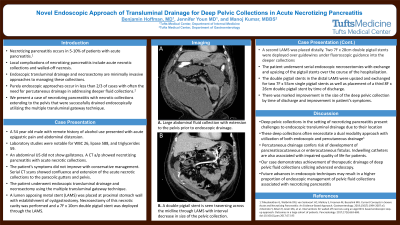
Using multiple transluminal gateway technique, a lumen apposing metal stent (LAMS) was placed at the proximal stomach wall with establishment of cystgastrostomy. A necrosectomy was performed and a 7F x 10 cm double pigtail stent was deployed through the LAMS. A second LAMS was placed distally and two 7F x 28 cm double pigtail stents were deployed over a guidewire under fluoroscopic guidance into the deeper pelvic collections. These stents were exchanged and upsized on subsequent necrosectomies. Interval abdominal imaging showed a significant decrease in the fluid collection size to 7.5 x 5.7 cm prior to discharge. Serially imaging demonstrated a continued decrease in collection size in the outpatient setting.
Discussion: Current management of acute necrotizing pancreatitis utilizes a step-up approach, relegating open necrosectomy as a last resort. Exclusive endoscopic approach for management is only achieved in 60% of patients. In remaining patients, adjunctive PCD is required. PCD confers risk of development of pancreaticocutaneous or enterocutaneous fistulas. Indwelling catheters are also associated with impaired quality of life for patients. This novel endoscopic approach resulted in marked improvement in deep fluid collections normally reserved for PCD. Future advances in endoscopic techniques may result in a higher proportion of endoscopic exclusivity in the management of fluid collections associated with necrotizing pancreatitis.

Figure: Figure 1. Computed tomography of the abdomen and pelvis demonstrating necrotizing pancreatitis with large fluid collection. A. Large abdominal fluid collection with extension to the pelvis prior to endoscopic drainage. B. A double pigtail stent is seen traversing across the midline through the lumen apposing metal stent with interval decrease in size of the deep pelvic collection.
Disclosures:
Benjamin Hoffman indicated no relevant financial relationships.
Jennifer Youn indicated no relevant financial relationships.
Manoj Kumar indicated no relevant financial relationships.
Benjamin E. Hoffman, MD, Jennifer Youn, MD, Manoj Kumar, MD. P1078 - Novel Endoscopic Approach of Transluminal Drainage for Deep Pelvic Collections in Acute Necrotizing Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
