Sunday Poster Session
Category: Interventional Endoscopy
P1081 - A Case of True Achalasia in the Context of Advanced Gastric Adenocarcinoma
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

David Okuampa, MD
Louisiana State University Health
Shreveport, LA
Presenting Author(s)
David Okuampa, MD1, Omar Khan, MD2, Qiang Cai, MD2
1Louisiana State University Health, Shreveport, LA; 2LSU Health, Shreveport, LA
Introduction: Achalasia is believed to result from the degeneration of the myenteric plexus, leading to the failure of relaxation of the lower esophageal sphincter and loss of peristalsis. While idiopathic achalasia has no known cause, various diseases are associated with secondary achalasia. Pseudoachalasia can present with similar manometric findings to achalasia but is associated with malignancy. Here, we present a unique case of a patient with true achalasia in the setting of gastric cancer.
Case Description/Methods: A 65-year-old African American male with a history of hypertension and a 50 pack-year smoking history presented to the endoscopy unit for an Esophageal Peroral Endoscopic Myotomy (E-POEM) procedure due to progressive dysphagia to solid and liquid food. Esophageal manometry confirmed type 1 achalasia.
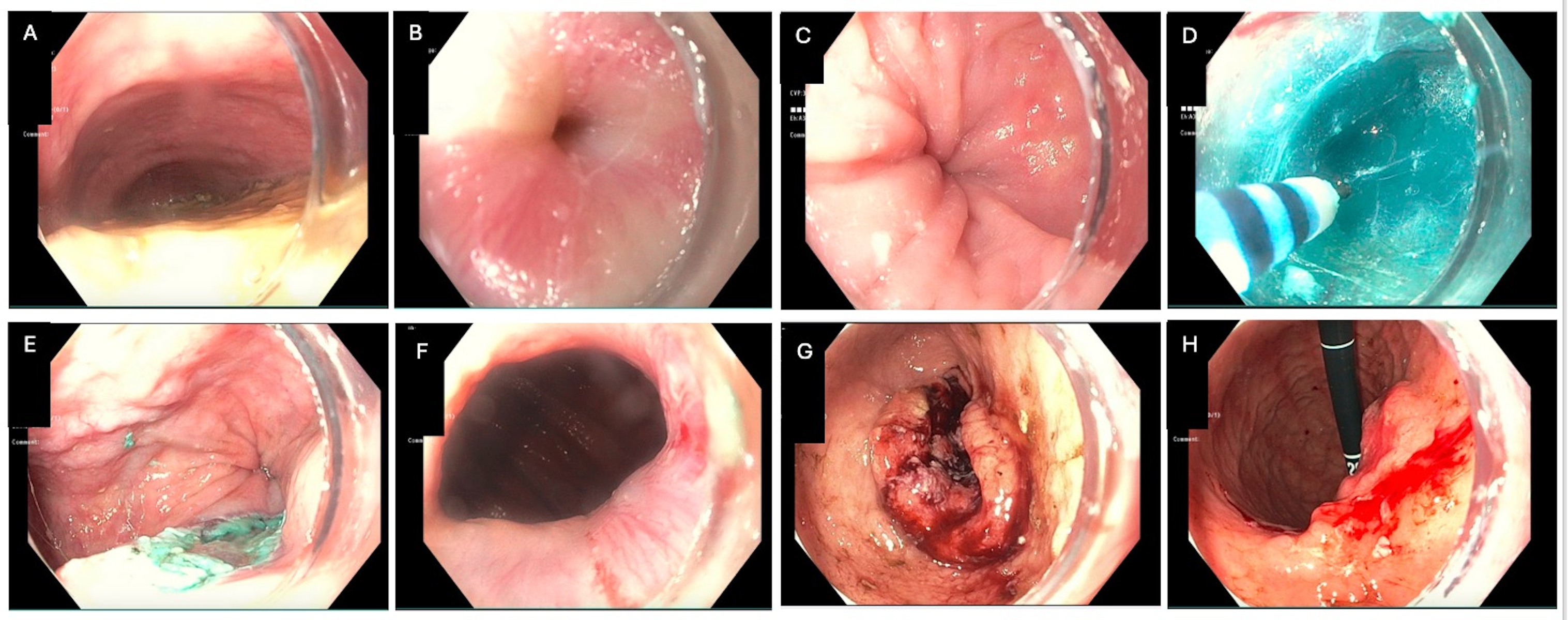
During the E-POEM, a malignant-appearing and ulcerated mass was noted, spanning from the lesser curvature to the antrum and pylorus (Figure 1G-H). Pathology reports and CT imaging confirmed Stage IV gastric adenocarcinoma. The patient’s dysphagia improved after the procedure.
Following an interdisciplinary discussion, it was determined that the patient’s prognosis was poor. Consequently, the patient and his family opted for palliative care.
Discussion: This patient's EGD revealed a normal GE junction following the E-POEM procedure. According to our literature review, this is the first documented case of true achalasia occurring in the context of gastric adenocarcinoma. The patient exhibited no symptoms other than dysphagia prior to the E-POEM, making the temporal relationship between type I achalasia and the onset of gastric adenocarcinoma unclear. Long-standing mucosal damage from achalasia is believed to potentially lead to esophageal cancer. Pseudoachalasia has been associated with cancers, typically gastric adenocarcinoma, that involve the GE junction by invading the myenteric nerve plexus. This case demonstrates that true achalasia can coexist with gastric adenocarcinoma that does not involve the GE junction, highlighting the need for careful differential diagnosis in similar clinical scenarios.
Disclosures:
David Okuampa, MD1, Omar Khan, MD2, Qiang Cai, MD2. P1081 - A Case of True Achalasia in the Context of Advanced Gastric Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Louisiana State University Health, Shreveport, LA; 2LSU Health, Shreveport, LA
Introduction: Achalasia is believed to result from the degeneration of the myenteric plexus, leading to the failure of relaxation of the lower esophageal sphincter and loss of peristalsis. While idiopathic achalasia has no known cause, various diseases are associated with secondary achalasia. Pseudoachalasia can present with similar manometric findings to achalasia but is associated with malignancy. Here, we present a unique case of a patient with true achalasia in the setting of gastric cancer.
Case Description/Methods: A 65-year-old African American male with a history of hypertension and a 50 pack-year smoking history presented to the endoscopy unit for an Esophageal Peroral Endoscopic Myotomy (E-POEM) procedure due to progressive dysphagia to solid and liquid food. Esophageal manometry confirmed type 1 achalasia.
During the E-POEM, a malignant-appearing and ulcerated mass was noted, spanning from the lesser curvature to the antrum and pylorus (Figure 1G-H). Pathology reports and CT imaging confirmed Stage IV gastric adenocarcinoma. The patient’s dysphagia improved after the procedure.
Following an interdisciplinary discussion, it was determined that the patient’s prognosis was poor. Consequently, the patient and his family opted for palliative care.
Discussion: This patient's EGD revealed a normal GE junction following the E-POEM procedure. According to our literature review, this is the first documented case of true achalasia occurring in the context of gastric adenocarcinoma. The patient exhibited no symptoms other than dysphagia prior to the E-POEM, making the temporal relationship between type I achalasia and the onset of gastric adenocarcinoma unclear. Long-standing mucosal damage from achalasia is believed to potentially lead to esophageal cancer. Pseudoachalasia has been associated with cancers, typically gastric adenocarcinoma, that involve the GE junction by invading the myenteric nerve plexus. This case demonstrates that true achalasia can coexist with gastric adenocarcinoma that does not involve the GE junction, highlighting the need for careful differential diagnosis in similar clinical scenarios.
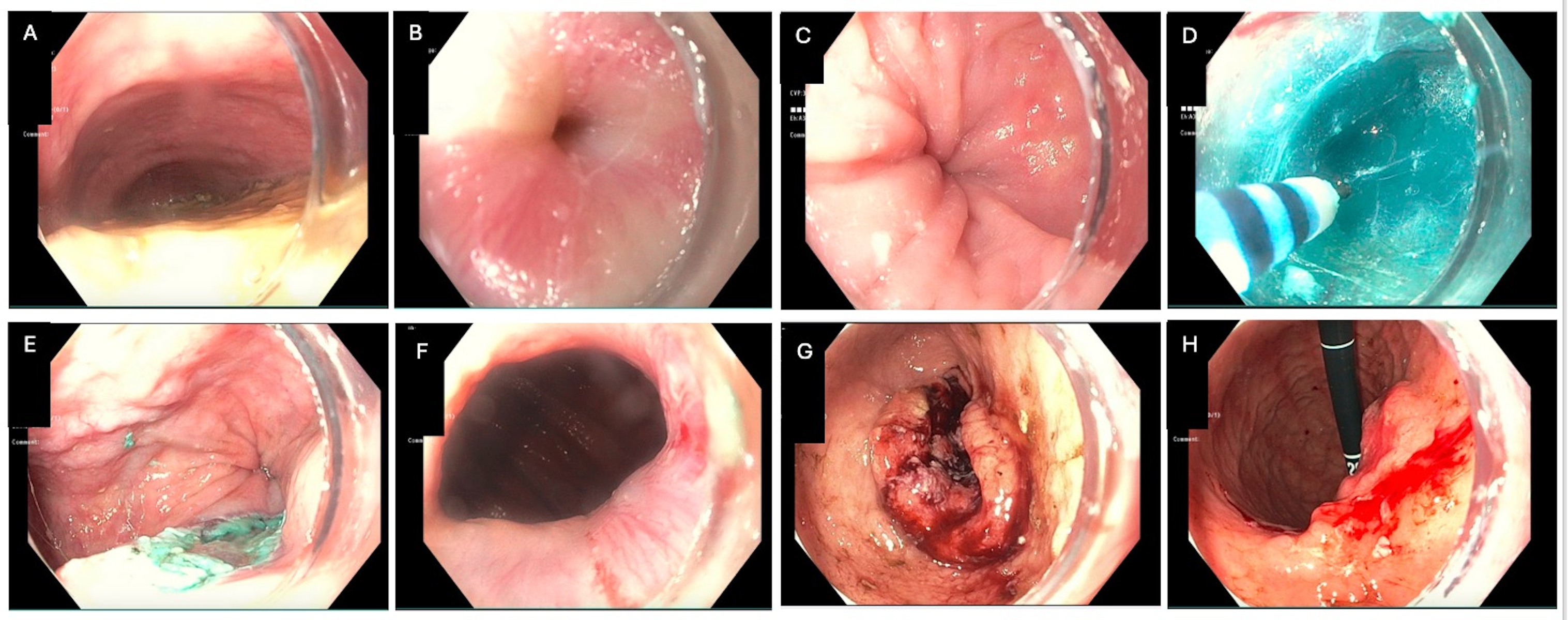
Figure: Figure 1A-C: Pre- E-POEM with significant amount of food content and narrowing of the GE junction
Figure 1D-F: Submucosal tunnel creation during E-POEM.
Figure 1G-H: Malignant appearing and ulcerative mass in lesser curvature, antrum, and pylorus (not traversable).
Figure 1D-F: Submucosal tunnel creation during E-POEM.
Figure 1G-H: Malignant appearing and ulcerative mass in lesser curvature, antrum, and pylorus (not traversable).
Disclosures:
David Okuampa indicated no relevant financial relationships.
Omar Khan indicated no relevant financial relationships.
Qiang Cai indicated no relevant financial relationships.
David Okuampa, MD1, Omar Khan, MD2, Qiang Cai, MD2. P1081 - A Case of True Achalasia in the Context of Advanced Gastric Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
