Sunday Poster Session
Category: IBD
P0992 - The Persistent Wound: Plasmablastic Lymphoma in a Perianal Fistula
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Salim C. Lutfallah, BS
LSU Health New Orleans School of Medicine
Metairie, LA
Presenting Author(s)
Salim C.. Lutfallah, BS1, John F. G.. Bobo, MD2, Rachna Jetly-Shridhar, MD, MPH2, Nisha Loganantharaj, MD2
1LSU Health New Orleans School of Medicine, Metairie, LA; 2LSU, New Orleans, LA
Introduction: Plasmablastic lymphoma (PBL) is a highly aggressive subtype of diffuse large B-cell lymphoma. While its incidence peaks within human immunodeficiency virus (HIV)-positive populations, a notable case in 2011 described PBL in an HIV-negative individual with a perianal fistula. PBL has since been described in various locations including the stomach, lungs, and bone marrow. Immune dysregulation plays a pivotal role in its development, evident by its strong association with HIV and Epstein-Barr Virus (EBV). PBL typically exhibits aggressive behavior and poor responsiveness to treatment, with a median overall survival of 9 months. To date, only 8 cases of PBL have been reported in HIV-negative patients with Crohn’s disease (CD). Here, we present a patient with ileocolonic and perianal CD, diagnosed with PBL based on fistula biopsies.
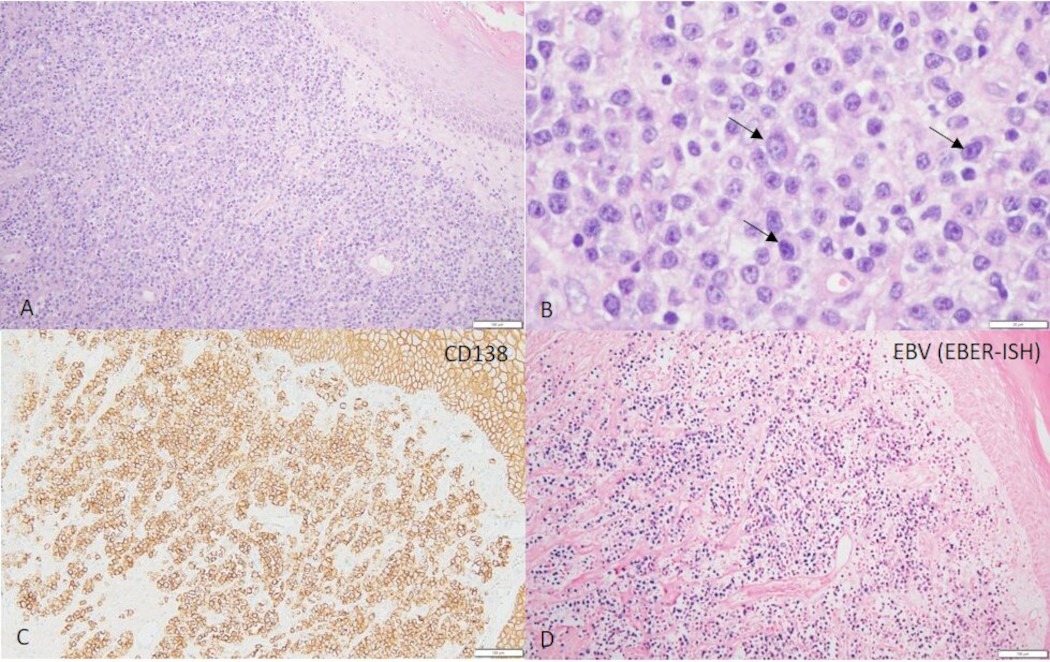
Case Description/Methods: A 54-year-old man presented with profuse rectal bleeding. In 2017, he was diagnosed with ileocolonic and perianal fistulizing CD. By 2020, he underwent a left lower quadrant diverting colostomy and developed a chronic gluteal wound, necessitating treatment with ertapenem and daptomycin. From 2017 to 2020, his CD had been managed with adalimumab and subsequently prednisone. At the time of presentation, he had been on prednisone 5 mg daily for over a year. Initial workup revealed an afebrile and hemodynamically stable patient with a hemoglobin of 8 g/dL. Colorectal surgery performed an exam under anesthesia, revealing multiple tracts without communication to the anus or rectum, alongside a small abscess. Biopsies of the fistulous tract confirmed PBL, characterized by dermal infiltrates of plasmablasts positive for CD56, CD138, kappa, and EBV. He is currently undergoing chemotherapy with V-EPOCH which includes bortezomib, etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin.
Discussion: Chronic immunosuppression significantly increases the risk of developing PBL. In this case, the prolonged use of prednisone and the chronic nature of his perianal fistulas likely contributed to the development of PBL. While it's possible that prior treatments with anti-TNF agonists may have contributed to PBL development, evidence of this relationship is not entirely clear due to potential confounding effects from immunomodulators such as azathioprine. This case highlights the importance of considering PBL in patients with persistent gluteal wounds and fistulas, particularly in the context of chronic prednisone use and immunosuppression.
Disclosures:
Salim C.. Lutfallah, BS1, John F. G.. Bobo, MD2, Rachna Jetly-Shridhar, MD, MPH2, Nisha Loganantharaj, MD2. P0992 - The Persistent Wound: Plasmablastic Lymphoma in a Perianal Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1LSU Health New Orleans School of Medicine, Metairie, LA; 2LSU, New Orleans, LA
Introduction: Plasmablastic lymphoma (PBL) is a highly aggressive subtype of diffuse large B-cell lymphoma. While its incidence peaks within human immunodeficiency virus (HIV)-positive populations, a notable case in 2011 described PBL in an HIV-negative individual with a perianal fistula. PBL has since been described in various locations including the stomach, lungs, and bone marrow. Immune dysregulation plays a pivotal role in its development, evident by its strong association with HIV and Epstein-Barr Virus (EBV). PBL typically exhibits aggressive behavior and poor responsiveness to treatment, with a median overall survival of 9 months. To date, only 8 cases of PBL have been reported in HIV-negative patients with Crohn’s disease (CD). Here, we present a patient with ileocolonic and perianal CD, diagnosed with PBL based on fistula biopsies.
Case Description/Methods: A 54-year-old man presented with profuse rectal bleeding. In 2017, he was diagnosed with ileocolonic and perianal fistulizing CD. By 2020, he underwent a left lower quadrant diverting colostomy and developed a chronic gluteal wound, necessitating treatment with ertapenem and daptomycin. From 2017 to 2020, his CD had been managed with adalimumab and subsequently prednisone. At the time of presentation, he had been on prednisone 5 mg daily for over a year. Initial workup revealed an afebrile and hemodynamically stable patient with a hemoglobin of 8 g/dL. Colorectal surgery performed an exam under anesthesia, revealing multiple tracts without communication to the anus or rectum, alongside a small abscess. Biopsies of the fistulous tract confirmed PBL, characterized by dermal infiltrates of plasmablasts positive for CD56, CD138, kappa, and EBV. He is currently undergoing chemotherapy with V-EPOCH which includes bortezomib, etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin.
Discussion: Chronic immunosuppression significantly increases the risk of developing PBL. In this case, the prolonged use of prednisone and the chronic nature of his perianal fistulas likely contributed to the development of PBL. While it's possible that prior treatments with anti-TNF agonists may have contributed to PBL development, evidence of this relationship is not entirely clear due to potential confounding effects from immunomodulators such as azathioprine. This case highlights the importance of considering PBL in patients with persistent gluteal wounds and fistulas, particularly in the context of chronic prednisone use and immunosuppression.
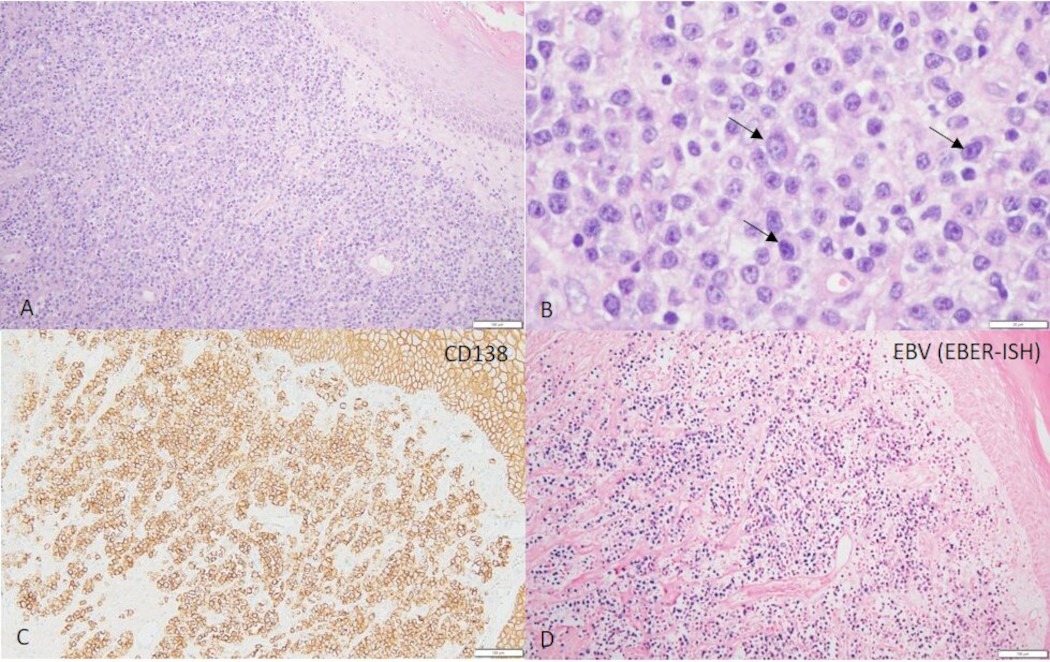
Figure: Figure legend: (A and B) Perianal fistulous tract biopsy section stained with hematoxylin and eosin stain, (A) low power view, (B) high power view; (C) Section stained with CD138; (D) Section stained with EBV (EBER-ISH). A dermal diffuse infiltrate of pleomorphic plasmacytoid cells with prominent nucleoli (B - arrows), positive for CD138 (C) and EBER-ISH (D).
Disclosures:
Salim Lutfallah indicated no relevant financial relationships.
John Bobo indicated no relevant financial relationships.
Rachna Jetly-Shridhar indicated no relevant financial relationships.
Nisha Loganantharaj: Abbvie – Speakers Bureau. Bristol Myers Squibb – Speakers Bureau. Eli Lilly – Advisory Committee/Board Member, Speakers Bureau. Takeda – Speakers Bureau.
Salim C.. Lutfallah, BS1, John F. G.. Bobo, MD2, Rachna Jetly-Shridhar, MD, MPH2, Nisha Loganantharaj, MD2. P0992 - The Persistent Wound: Plasmablastic Lymphoma in a Perianal Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

