Sunday Poster Session
Category: IBD
P1003 - A Case of May-Thurner Syndrome in a Patient With Active Crohn’s Colitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Navila Sharif, MD
Emory University School of Medicine
Atlanta, GA
Presenting Author(s)
Navila Sharif, MD, Rishi Das, MD, MPH, Tanvi Dhere, MD
Emory University School of Medicine, Atlanta, GA
Introduction: May-Thurner syndrome is a compressive vascular condition that can lead to acute deep vein thrombosis (DVT) in susceptible patients. We present a unique case of a female patient with extensive lower extremity DVT secondary to May-Thurner syndrome in the setting of active Crohn’s disease.
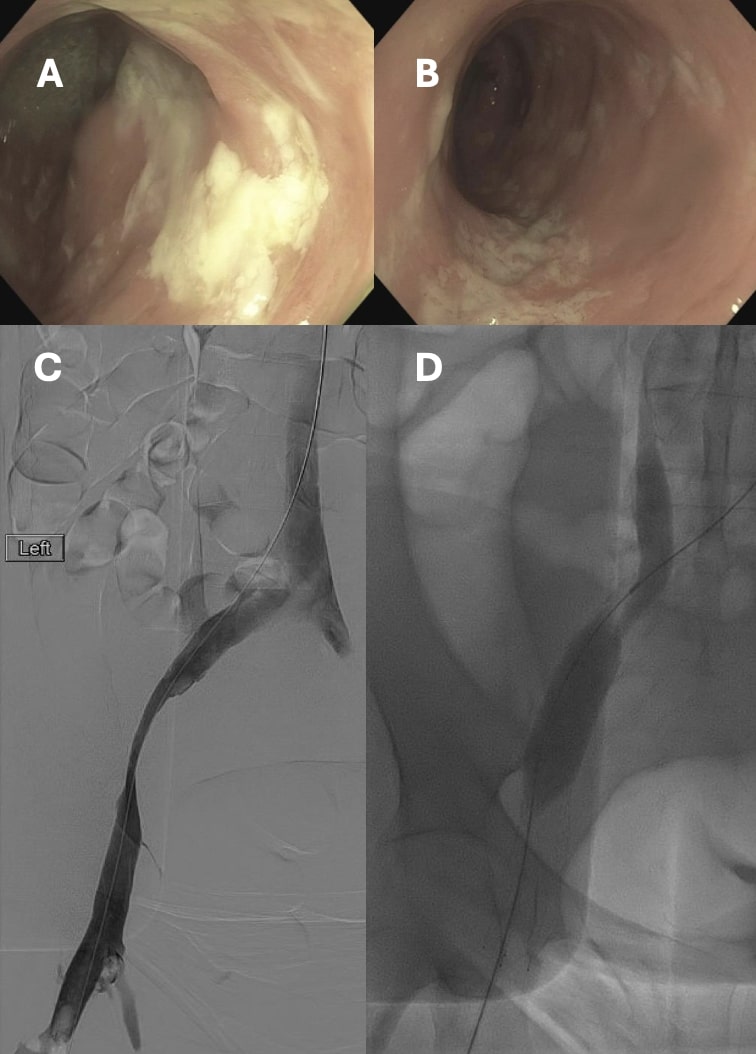
Case Description/Methods: A 39-year-old woman with a history of seronegative inflammatory arthritis on etanercept, uterine fibroids, and anemia presented with subacute bloody diarrhea over a two-month period. She also complained of a month of acute right eye pain and two weeks of left leg swelling and pain. CT abdomen and pelvis showed colonic wall thickening extending from distal transverse colon to the rectum consistent with proctocolitis. C-reactive protein (CRP) was elevated to 170 mg/L. Imaging and overall clinical picture including anterior uveitis and patient’s autoimmune history were concerning for a new diagnosis of inflammatory bowel disease (IBD). This was confirmed by colonoscopy showing moderate to severe colonic ulcerations with intervening normal mucosa, and final pathology revealing chronic active colitis with multiple granulomas consistent with Crohn’s disease. Patient was also found to have a new occlusive left iliofemoral DVT. She had no other predisposing factors other than severe Crohn’s colitis for developing the DVT. She underwent thrombectomy with stent placement that revealed significant clot burden and was noted to have high grade stenosis of the left external iliac and left common iliac vein consistent with May-Thurner physiology.
Discussion: May-Thurner Syndrome, also known as iliac vein compression syndrome (IVCS), is a vascular disorder that results from compression of the left iliac vein between the right iliac artery and the vertebrae, resulting in venous outflow obstruction. Risk factors include female sex and personal history of hypercoagulable disorder. Our patient was found to have a significantly sized venous thromboembolism (VTE) without classic risk factors but had a new diagnosis of severe Crohn’s colitis- which independently increases risk of VTE, particularly during active disease, but has not previously been linked with May-Thurner syndrome. This case highlights the importance of considering thrombotic complications associated with IBD in patients that present with a new diagnosis or flare.
Disclosures:
Navila Sharif, MD, Rishi Das, MD, MPH, Tanvi Dhere, MD. P1003 - A Case of May-Thurner Syndrome in a Patient With Active Crohn’s Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Emory University School of Medicine, Atlanta, GA
Introduction: May-Thurner syndrome is a compressive vascular condition that can lead to acute deep vein thrombosis (DVT) in susceptible patients. We present a unique case of a female patient with extensive lower extremity DVT secondary to May-Thurner syndrome in the setting of active Crohn’s disease.
Case Description/Methods: A 39-year-old woman with a history of seronegative inflammatory arthritis on etanercept, uterine fibroids, and anemia presented with subacute bloody diarrhea over a two-month period. She also complained of a month of acute right eye pain and two weeks of left leg swelling and pain. CT abdomen and pelvis showed colonic wall thickening extending from distal transverse colon to the rectum consistent with proctocolitis. C-reactive protein (CRP) was elevated to 170 mg/L. Imaging and overall clinical picture including anterior uveitis and patient’s autoimmune history were concerning for a new diagnosis of inflammatory bowel disease (IBD). This was confirmed by colonoscopy showing moderate to severe colonic ulcerations with intervening normal mucosa, and final pathology revealing chronic active colitis with multiple granulomas consistent with Crohn’s disease. Patient was also found to have a new occlusive left iliofemoral DVT. She had no other predisposing factors other than severe Crohn’s colitis for developing the DVT. She underwent thrombectomy with stent placement that revealed significant clot burden and was noted to have high grade stenosis of the left external iliac and left common iliac vein consistent with May-Thurner physiology.
Discussion: May-Thurner Syndrome, also known as iliac vein compression syndrome (IVCS), is a vascular disorder that results from compression of the left iliac vein between the right iliac artery and the vertebrae, resulting in venous outflow obstruction. Risk factors include female sex and personal history of hypercoagulable disorder. Our patient was found to have a significantly sized venous thromboembolism (VTE) without classic risk factors but had a new diagnosis of severe Crohn’s colitis- which independently increases risk of VTE, particularly during active disease, but has not previously been linked with May-Thurner syndrome. This case highlights the importance of considering thrombotic complications associated with IBD in patients that present with a new diagnosis or flare.
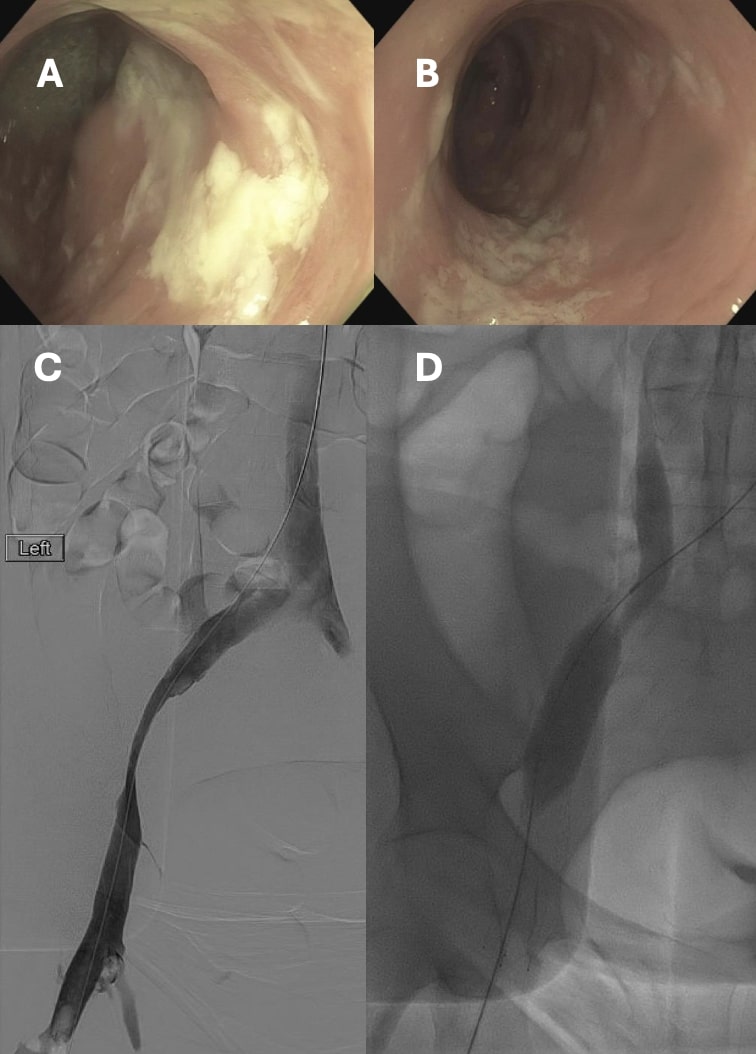
Figure: A and B: Endoscopic findings of moderate to severe colonic
ulcerations
C and D: Lower extremity venogram showing stenosis of L external iliac
vein and L common iliac vein where R common iliac artery
crosses over the vein
ulcerations
C and D: Lower extremity venogram showing stenosis of L external iliac
vein and L common iliac vein where R common iliac artery
crosses over the vein
Disclosures:
Navila Sharif indicated no relevant financial relationships.
Rishi Das indicated no relevant financial relationships.
Tanvi Dhere indicated no relevant financial relationships.
Navila Sharif, MD, Rishi Das, MD, MPH, Tanvi Dhere, MD. P1003 - A Case of May-Thurner Syndrome in a Patient With Active Crohn’s Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
