Sunday Poster Session
Category: IBD
P1004 - Ulcerative Colitis or Not? A Case of Dysplasia, Gastrointestinal Bleeding and Juvenile Polyposis in a 27-Year-Old
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Stephanie Ren, MD
New York University Langone Health Long Island
Mineola, NY
Presenting Author(s)
Stephanie Ren, MD1, Tianyu She, DO1, Harry He, MD1, Matthew Symer, MD2, Seymour Katz, MD3
1New York University Langone Health Long Island, Mineola, NY; 2NYU Grossman Long Island School of Medicine, New Hyde Park, NY; 3NYU Grossman School of Medicine, New Hyde Park, NY
Introduction: Patients with juvenile polyposis syndrome (JPS) typically present with polyps that initially appear benign but harbor an increased risk of gastrointestinal cancer. A patient presenting with history of ulcerative colitis (UC) and underlying undiagnosed JPS can present with diagnostic difficulty as there is significant overlap in associated symptoms. Moreover, both conditions are independently associated with increased cancer risk.
Case Description/Methods: A 27-year-old male with past medical history of noncompliant UC diagnosed at age 14 was found to be with severe anemia secondary to multiple maroon-colored bowel movements. CT angiography demonstrated active extravasation and mild bowel wall thickening of the rectosigmoid colon. He received 3 units of packed red blood cells and iron supplementation. Endoscopy revealed three gastric hyperplastic polyps and numerous juvenile and inflammatory polyps throughout the colon, largest measuring 80 mm, with indeterminate dysplasia in the ascending colon, low grade in the descending colon, and high grade in the rectum with p53 null expression and loss of SMAD4 expression throughout.
MRI of the rectum revealed active inflammation in addition to a primary 4.9 x 5.9 x 4.1 cm polypoid T3a tumor with a superior rectal lymph node without evidence of carcinoma on biopsy. The patient underwent a proctocolectomy with ileal pouch-anal anastomosis and diverting loop ileostomy and subsequent loop ileostomy reversal was planned.
Discussion: Both JPS and UC can present similarly symptomatically and histologically. The median age of colorectal carcinoma in JPS is reported at 41 years, yet this patient is 27 and already exhibits evidence of high-grade dysplasia. The inflammation from uncontrolled UC was initially thought to be contributory but, there was limited inflammation on direct visualization and from mucosal biopsies of the left colon and rectum. However, biopsies of the polyps themselves had juvenile and inflammatory findings histologically. Thus, the inflammatory burden and dysplasia that was observed is likely secondary to JPS than from UC.
To date, there have been no studies that quantify the risk of cancer in patients with both JPS and UC and a potential accelerated progression to malignancy. The subsequent increased risk may require shorter time intervals of surveillance as well as anti-inflammatory therapy. In addition, close attention and a wide differential must be cast for these patients with IBD, as this originally presented as a UC flare mimicker.

Disclosures:
Stephanie Ren, MD1, Tianyu She, DO1, Harry He, MD1, Matthew Symer, MD2, Seymour Katz, MD3. P1004 - Ulcerative Colitis or Not? A Case of Dysplasia, Gastrointestinal Bleeding and Juvenile Polyposis in a 27-Year-Old, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York University Langone Health Long Island, Mineola, NY; 2NYU Grossman Long Island School of Medicine, New Hyde Park, NY; 3NYU Grossman School of Medicine, New Hyde Park, NY
Introduction: Patients with juvenile polyposis syndrome (JPS) typically present with polyps that initially appear benign but harbor an increased risk of gastrointestinal cancer. A patient presenting with history of ulcerative colitis (UC) and underlying undiagnosed JPS can present with diagnostic difficulty as there is significant overlap in associated symptoms. Moreover, both conditions are independently associated with increased cancer risk.
Case Description/Methods: A 27-year-old male with past medical history of noncompliant UC diagnosed at age 14 was found to be with severe anemia secondary to multiple maroon-colored bowel movements. CT angiography demonstrated active extravasation and mild bowel wall thickening of the rectosigmoid colon. He received 3 units of packed red blood cells and iron supplementation. Endoscopy revealed three gastric hyperplastic polyps and numerous juvenile and inflammatory polyps throughout the colon, largest measuring 80 mm, with indeterminate dysplasia in the ascending colon, low grade in the descending colon, and high grade in the rectum with p53 null expression and loss of SMAD4 expression throughout.
MRI of the rectum revealed active inflammation in addition to a primary 4.9 x 5.9 x 4.1 cm polypoid T3a tumor with a superior rectal lymph node without evidence of carcinoma on biopsy. The patient underwent a proctocolectomy with ileal pouch-anal anastomosis and diverting loop ileostomy and subsequent loop ileostomy reversal was planned.
Discussion: Both JPS and UC can present similarly symptomatically and histologically. The median age of colorectal carcinoma in JPS is reported at 41 years, yet this patient is 27 and already exhibits evidence of high-grade dysplasia. The inflammation from uncontrolled UC was initially thought to be contributory but, there was limited inflammation on direct visualization and from mucosal biopsies of the left colon and rectum. However, biopsies of the polyps themselves had juvenile and inflammatory findings histologically. Thus, the inflammatory burden and dysplasia that was observed is likely secondary to JPS than from UC.
To date, there have been no studies that quantify the risk of cancer in patients with both JPS and UC and a potential accelerated progression to malignancy. The subsequent increased risk may require shorter time intervals of surveillance as well as anti-inflammatory therapy. In addition, close attention and a wide differential must be cast for these patients with IBD, as this originally presented as a UC flare mimicker.

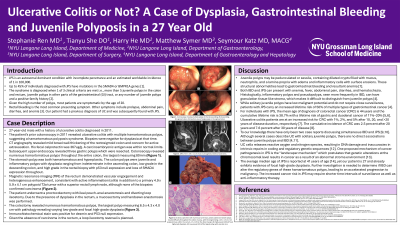
Figure: Colonoscopy showing multiple polyps in the (A) ascending, (B) descending, (C) sigmoid colon. (D) Another view of single polyp in the sigmoid colon.
Disclosures:
Stephanie Ren indicated no relevant financial relationships.
Tianyu She indicated no relevant financial relationships.
Harry He indicated no relevant financial relationships.
Matthew Symer indicated no relevant financial relationships.
Seymour Katz indicated no relevant financial relationships.
Stephanie Ren, MD1, Tianyu She, DO1, Harry He, MD1, Matthew Symer, MD2, Seymour Katz, MD3. P1004 - Ulcerative Colitis or Not? A Case of Dysplasia, Gastrointestinal Bleeding and Juvenile Polyposis in a 27-Year-Old, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
