Sunday Poster Session
Category: IBD
P0911 - Recurrence Patterns in Crohn's Disease Patients With End Ostomies: Insights From the Cleveland Clinic IBD Ostomy Research Registry
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

Wesam Aleyadeh, MD
Cleveland Clinic Akron General
Akron, OH
Presenting Author(s)
Wesam Aleyadeh, MD1, Raj Jessica Thomas, MD1, Katherine Falloon, MD2, Catherine Larson, MS3, Yueqi (Renee) Wu, MPH4, Qijun Yang, MS5, Florian Rieder, MD6, Suha Abushamma, MD5
1Cleveland Clinic Akron General, Akron, OH; 2Cleveland Clinic Foundation, Shaker Heights, OH; 3Cleveland Clinic Foundation, Cleveland, OH; 4Cleveland Clinic Lerner Research Institute, Cleveland Heights, OH; 5Cleveland Clinic, Cleveland, OH; 6Digestive Diseases and Surgery Institute; Lerner Research Institute, Program for Global Translational Inflammatory Bowel Diseases; Cleveland Clinic Foundation, Cleveland, OH
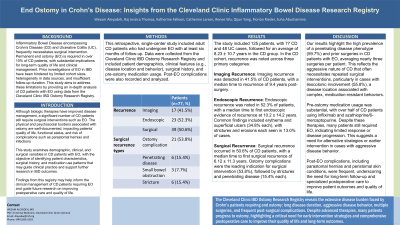
Introduction: Inflammatory Bowel Disease (IBD) and its two distinct forms, ulcerative colitis (UC) and Crohn's disease (CD), often result in the need for surgical intervention. Creation of a permanent end ostomy (EO) is ultimately required in 8% of UC and over 10% of CD patients, presenting a significant impact on patient quality of life and clinical management. Previous studies on IBD patients with EO have been limited by small sample sizes, heterogeneous data, and short follow-up time. This study aims to provide a comprehensive analysis of recurrence patterns in CD patients with EO utilizing data from the Cleveland Clinic IBD Ostomy Research Registry.
Methods: This retrospective single-institution study used a comprehensive registry of IBD patients aged 18 or older who had an EO created and at least six months of follow-up. Data was collected on different demographic, clinical, and surgical variables. Statistical analyses were performed using R Studio.
Results: 125 patients (77 CD, 48 UC) were included. In the CD cohort, 75 (97.4%) had end-ileostomy, while 2 had end-colostomy. The mean time from ostomy surgery to the last follow-up was 8.23 (±10.7). The mean age at diagnosis was 28.4 (±16.9) years, and the mean age at ostomy surgery was 41.4 (±15.5) years. The median time from diagnosis to surgery was 13.0 (±10.5) years. Recurrence was observed on follow-up imaging in 17 (41.5%) of patients at a median of 9.40 years post-surgery to the first evidence of recurrence on imaging. Endoscopic recurrence was noted in 23 (52.3%) of patients at a median of 10.2 (±14.2) years post-surgery. The endoscopy findings were most commonly erythema and superficial ulcers in 8 (34.8%) patients each, followed by erosions and strictures in 3 (13.0%) patients each. Surgical recurrence was noted in 39 (50.6%) patients, with ostomy complications being the most common indication for surgery in 21 (53.8%) patients followed by strictures and penetrating disease in 6 (15.4%) patients each. The median time to the first recurrence was 6.12 (±11.3) years.
Discussion: This study provides a detailed analysis of recurrence patterns in CD patients with end ostomies, highlighting significant rates of imaging, endoscopic, and surgical recurrences. The findings from this registry emphasize the need for long-term monitoring and targeted management strategies to address recurrence in this population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Wesam Aleyadeh, MD1, Raj Jessica Thomas, MD1, Katherine Falloon, MD2, Catherine Larson, MS3, Yueqi (Renee) Wu, MPH4, Qijun Yang, MS5, Florian Rieder, MD6, Suha Abushamma, MD5. P0911 - Recurrence Patterns in Crohn's Disease Patients With End Ostomies: Insights From the Cleveland Clinic IBD Ostomy Research Registry, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Akron General, Akron, OH; 2Cleveland Clinic Foundation, Shaker Heights, OH; 3Cleveland Clinic Foundation, Cleveland, OH; 4Cleveland Clinic Lerner Research Institute, Cleveland Heights, OH; 5Cleveland Clinic, Cleveland, OH; 6Digestive Diseases and Surgery Institute; Lerner Research Institute, Program for Global Translational Inflammatory Bowel Diseases; Cleveland Clinic Foundation, Cleveland, OH
Introduction: Inflammatory Bowel Disease (IBD) and its two distinct forms, ulcerative colitis (UC) and Crohn's disease (CD), often result in the need for surgical intervention. Creation of a permanent end ostomy (EO) is ultimately required in 8% of UC and over 10% of CD patients, presenting a significant impact on patient quality of life and clinical management. Previous studies on IBD patients with EO have been limited by small sample sizes, heterogeneous data, and short follow-up time. This study aims to provide a comprehensive analysis of recurrence patterns in CD patients with EO utilizing data from the Cleveland Clinic IBD Ostomy Research Registry.
Methods: This retrospective single-institution study used a comprehensive registry of IBD patients aged 18 or older who had an EO created and at least six months of follow-up. Data was collected on different demographic, clinical, and surgical variables. Statistical analyses were performed using R Studio.
Results: 125 patients (77 CD, 48 UC) were included. In the CD cohort, 75 (97.4%) had end-ileostomy, while 2 had end-colostomy. The mean time from ostomy surgery to the last follow-up was 8.23 (±10.7). The mean age at diagnosis was 28.4 (±16.9) years, and the mean age at ostomy surgery was 41.4 (±15.5) years. The median time from diagnosis to surgery was 13.0 (±10.5) years. Recurrence was observed on follow-up imaging in 17 (41.5%) of patients at a median of 9.40 years post-surgery to the first evidence of recurrence on imaging. Endoscopic recurrence was noted in 23 (52.3%) of patients at a median of 10.2 (±14.2) years post-surgery. The endoscopy findings were most commonly erythema and superficial ulcers in 8 (34.8%) patients each, followed by erosions and strictures in 3 (13.0%) patients each. Surgical recurrence was noted in 39 (50.6%) patients, with ostomy complications being the most common indication for surgery in 21 (53.8%) patients followed by strictures and penetrating disease in 6 (15.4%) patients each. The median time to the first recurrence was 6.12 (±11.3) years.
Discussion: This study provides a detailed analysis of recurrence patterns in CD patients with end ostomies, highlighting significant rates of imaging, endoscopic, and surgical recurrences. The findings from this registry emphasize the need for long-term monitoring and targeted management strategies to address recurrence in this population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Wesam Aleyadeh indicated no relevant financial relationships.
Raj Jessica Thomas indicated no relevant financial relationships.
Katherine Falloon: Janssen – Advisory Committee/Board Member. Pfizer – Grant/Research Support.
Catherine Larson indicated no relevant financial relationships.
Yueqi (Renee) Wu indicated no relevant financial relationships.
Qijun Yang indicated no relevant financial relationships.
Florian Rieder: 89Bio – Consultant. AbbVie – Consultant, Grant/Research Support. Adiso – Consultant. Adnovate – Consultant. Agomab – Consultant. Allergan – Advisory Committee/Board Member, Consultant. Arena – Advisory Committee/Board Member, Consultant. AstraZeneca – Advisory Committee/Board Member, Consultant. Bausch & Lomb – Consultant. Boehringer Ingelheim – Advisory Committee/Board Member, Consultant, Grant/Research Support. CDISC – Consultant. Celgene/BMS – Advisory Committee/Board Member, Consultant, Grant/Research Support. Celltrion – Consultant. Celsius – Consultant. Cowen – Consultant. Eugit – Consultant. Ferring – Consultant. Galapagos – Consultant. Galmed – Consultant. Genentech – Advisory Committee/Board Member, Consultant. Gilead – Advisory Committee/Board Member, Consultant, Grant/Research Support. Gossamer – Consultant. Granite – Consultant. Guidepoint – Consultant. Helmsley – Consultant. Horizon Therapeutics – Consultant. Image Analysis Limited – Consultant. Index Pharma – Consultant. Jannsen – Consultant. Koutif – Consultant. Landos – Consultant. Mestag – Consultant. Metacrine – Consultant. Mirum – Consultant. Mopec – Consultant. Morphic – Consultant. Myka Labs – Consultant. Organovo – Consultant. Origo – Consultant. Palisade Bio – Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Grant/Research Support. Pliant – Consultant. Prometheus Biosciences – Advisory Committee/Board Member, Consultant. Receptos – Consultant. RedX – Advisory Committee/Board Member, Consultant. Roche – Advisory Committee/Board Member, Consultant. Samsung – Advisory Committee/Board Member, Consultant. Sanofi – Consultant. Surmodics – Consultant. Surrozen – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support. Techlab – Consultant. Teva – Consultant. Theravance – Consultant. Thetis – Consultant. Trix Bio – Consultant. UCB – Advisory Committee/Board Member, Consultant, Grant/Research Support. Ysios – Consultant.
Suha Abushamma indicated no relevant financial relationships.
Wesam Aleyadeh, MD1, Raj Jessica Thomas, MD1, Katherine Falloon, MD2, Catherine Larson, MS3, Yueqi (Renee) Wu, MPH4, Qijun Yang, MS5, Florian Rieder, MD6, Suha Abushamma, MD5. P0911 - Recurrence Patterns in Crohn's Disease Patients With End Ostomies: Insights From the Cleveland Clinic IBD Ostomy Research Registry, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
