Sunday Poster Session
Category: IBD
P0916 - Prophylaxis for Venous Thromboembolism Remains Low in Patients Admitted With Severe UC in the Community Setting
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Vivek V. Jasti, MD
OhioHealth Riverside Methodist Hospital
Columbus, OH
Presenting Author(s)
Vivek V. Jasti, MD1, Kim Jordan, MD2, Arun K.. Tewari, PhD3, David Y. Lo, MD4, Shail Govani, MD, MSc5
1OhioHealth Riverside Methodist Hospital, Columbus, OH; 2OhioHealth Riverside Methodist Hospital, Powell, OH; 3OhioHealth, Columbus, OH; 4Ohio Gastroenterology Group, New Albany, OH; 5Ohio Gastroenterology Group, Columbus, OH
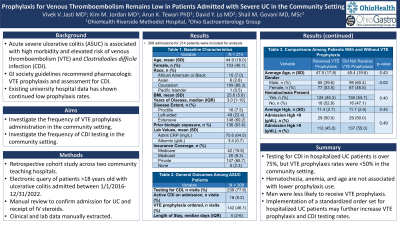
Introduction: Acute severe ulcerative colitis (ASUC) is a medical emergency associated with high morbidity. Hospitalized patients with ASUC are at increased risk of venous thromboembolism (VTE) and Clostridioides difficile infection (CDI). Gastroenterology society guidelines recommend pharmacologic VTE prophylaxis and assessment for CDI. Despite these guidelines, VTE prophylaxis rates in prior academic center studies remain low. In this retrospective study, we aimed to identify the frequency of administration of VTE prophylaxis and CDI testing in a community teaching hospital setting.
Methods: Medical records of a large community teaching hospital system in the United States were queried for hospitalizations for UC based on ICD10 codes between 1/1/2016 and 12/31/2022. Manual review verified that UC was the primary reason for admission. Relevant demographic and clinical data were gathered along with data on VTE prophylaxis administration and CDI testing. Categorical values were compared with chi-square testing while numerical values were compared with the Student’s t-test.
Results: A total of 308 hospitalizations for 214 individuals were identified. The average age was 44.9 ± 18.0 years and 103 (48.1%) were female. The median years of disease was 3.0 [IQR: 1-10]; 148 (69.2%) had disease proximal to the splenic flexure and 136 (63.6%) had either current or prior biologic exposure. Testing for CDI was ordered in 239 visits (77.6%). Prophylaxis for VTE was ordered in only 142 visits (46.1%). VTE prophylaxis was not significantly lower in patients presenting with hematochezia versus those without hematochezia (45.3% vs. 52.9%, respectively, p=0.40). The average admission hemoglobin did not differ between patients receiving prophylaxis and those without prophylaxis (11.4g/dL vs. 11.7g/dL, p=0.45). Males were less likely to receive VTE prophylaxis (39.6%) versus female (53.5%), p=0.02. Average age did not differ between patients receiving prophylaxis and those not receiving prophylaxis (47.0 vs. 45.4, p=0.43).
Discussion: While testing for CDI in patients hospitalized with UC is frequent, rates of VTE prophylaxis remains below 50% in the community hospital setting. Hematochezia and anemia do not appear to be associated with lower rates of VTE prophylaxis use. Further studies of the reasons behind low VTE prophylaxis utilization are necessary. Implementation of a standardized order set may further increase VTE prophylaxis and CDI testing rates in this patient population.
Disclosures:
Vivek V. Jasti, MD1, Kim Jordan, MD2, Arun K.. Tewari, PhD3, David Y. Lo, MD4, Shail Govani, MD, MSc5. P0916 - Prophylaxis for Venous Thromboembolism Remains Low in Patients Admitted With Severe UC in the Community Setting, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1OhioHealth Riverside Methodist Hospital, Columbus, OH; 2OhioHealth Riverside Methodist Hospital, Powell, OH; 3OhioHealth, Columbus, OH; 4Ohio Gastroenterology Group, New Albany, OH; 5Ohio Gastroenterology Group, Columbus, OH
Introduction: Acute severe ulcerative colitis (ASUC) is a medical emergency associated with high morbidity. Hospitalized patients with ASUC are at increased risk of venous thromboembolism (VTE) and Clostridioides difficile infection (CDI). Gastroenterology society guidelines recommend pharmacologic VTE prophylaxis and assessment for CDI. Despite these guidelines, VTE prophylaxis rates in prior academic center studies remain low. In this retrospective study, we aimed to identify the frequency of administration of VTE prophylaxis and CDI testing in a community teaching hospital setting.
Methods: Medical records of a large community teaching hospital system in the United States were queried for hospitalizations for UC based on ICD10 codes between 1/1/2016 and 12/31/2022. Manual review verified that UC was the primary reason for admission. Relevant demographic and clinical data were gathered along with data on VTE prophylaxis administration and CDI testing. Categorical values were compared with chi-square testing while numerical values were compared with the Student’s t-test.
Results: A total of 308 hospitalizations for 214 individuals were identified. The average age was 44.9 ± 18.0 years and 103 (48.1%) were female. The median years of disease was 3.0 [IQR: 1-10]; 148 (69.2%) had disease proximal to the splenic flexure and 136 (63.6%) had either current or prior biologic exposure. Testing for CDI was ordered in 239 visits (77.6%). Prophylaxis for VTE was ordered in only 142 visits (46.1%). VTE prophylaxis was not significantly lower in patients presenting with hematochezia versus those without hematochezia (45.3% vs. 52.9%, respectively, p=0.40). The average admission hemoglobin did not differ between patients receiving prophylaxis and those without prophylaxis (11.4g/dL vs. 11.7g/dL, p=0.45). Males were less likely to receive VTE prophylaxis (39.6%) versus female (53.5%), p=0.02. Average age did not differ between patients receiving prophylaxis and those not receiving prophylaxis (47.0 vs. 45.4, p=0.43).
Discussion: While testing for CDI in patients hospitalized with UC is frequent, rates of VTE prophylaxis remains below 50% in the community hospital setting. Hematochezia and anemia do not appear to be associated with lower rates of VTE prophylaxis use. Further studies of the reasons behind low VTE prophylaxis utilization are necessary. Implementation of a standardized order set may further increase VTE prophylaxis and CDI testing rates in this patient population.
Disclosures:
Vivek Jasti indicated no relevant financial relationships.
Kim Jordan indicated no relevant financial relationships.
Arun Tewari indicated no relevant financial relationships.
David Lo: Abbvie – Speakers Bureau. QOL – Speakers Bureau.
Shail Govani: Abbvie – Speakers Bureau. Bristol Meyers Squibb – Speakers Bureau.
Vivek V. Jasti, MD1, Kim Jordan, MD2, Arun K.. Tewari, PhD3, David Y. Lo, MD4, Shail Govani, MD, MSc5. P0916 - Prophylaxis for Venous Thromboembolism Remains Low in Patients Admitted With Severe UC in the Community Setting, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
