Sunday Poster Session
Category: IBD
P0927 - Impact of Malnutrition on Outcomes of Patients With Inflammatory Bowel Disease Hospitalized for Gastrointestinal Bleeding: A Propensity Score-Matched Study From a U.S. Collaborative Network
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Karecia Byfield, MBBS
Albert Einstein Medical Center
Philadelphia, PA
Presenting Author(s)
Karecia Byfield, MBBS1, Phuuwadith Wattanachayakul, MD1, Nino Gudushauri, MD2, Tinsae Anebo, MD1, Colton F. Jones, MBBS1, Fnu Deepali, MD3, Megan Johnson, MBBS4, Elvis Obomanu, MBBS5, Carlo Gabriel C. Casipit, MD1, Jordan Carty, MD1, Kevin Robinson, MD1, James Walter, MD6
1Albert Einstein Medical Center, Philadelphia, PA; 2Jefferson Einstein Hospital, Philadelphia, PA; 3Einstein Medical Center, Philadelphia, PA; 4Spanish Town Hospital, Kingston, Saint Andrew, Jamaica; 5Jefferson-Einstein Hospital, Philadelphia, PA; 6Einstein Healthcare Network, Philadelphia, PA
Introduction: Recent data highlight the complex interplay between malnutrition and inflammatory bowel disease (IBD), leading to adverse outcomes such as increased disease activity, poor therapy response, and diminished quality of life. However, the impact of malnutrition on patients with Crohn’s disease or ulcerative colitis hospitalized for gastrointestinal bleeding (GIB) remains unclear.
Methods: Data from the US Collaborative Network-TriNetX was used to evaluate the impact of malnutrition on IBD patients hospitalized for GIB. Patients were classified into two cohorts: those with malnutrition and those without as identified by the relevant ICD-10 codes. The malnutrition cohort was propensity score-matched with the control group based on age, sex, race, and comorbidities. Patients were then followed for 30 days post-hospitalization to assess outcomes including mortality, hypovolemic shock, perforation, ICU admission, need for transfusion, and endoscopic procedures.
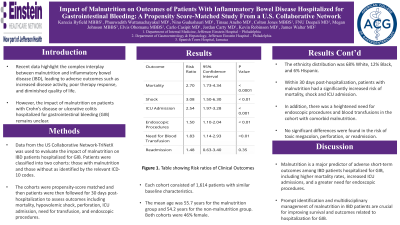
Results: After propensity score matching, each cohort consisted of 1,614 patients with similar baseline characteristics. The mean age was 55.7 years for the malnutrition group and 54.2 years for the non-malnutrition group. Both cohorts were 46% female. The ethnicity distribution was 68% White, 12% Black, and 6% Hispanic. Within 30 days post-hospitalization, patients with malnutrition had a significantly increased risk of all-cause mortality (RR: 2.7, 95% CI: 1.73-4.34, P< 0.0001), shock (RR: 3.08, 95% CI: 1.50-6.30, P< 0.01), and ICU admission (RR: 2.54, 95% CI: 1.97-3.28, P< 0.001). In addition, heightened risk for endoscopic procedures (RR: 1.5, 95% CI: 1.10-2.04, P< 0.01) and blood transfusions (RR: 1.83, 95% CI: 1.14-2.93, P=0.01) was found in the cohort with malnutrition compared to the cohort without. No significant differences were found in the risk of toxic megacolon, perforation, or readmission.
Discussion: Our study found that malnutrition is a major predictor of adverse short-term outcomes among IBD patients hospitalized for GIB, including higher mortality rates, increased ICU admissions, and a greater need for endoscopic procedures. Prompt identification and multidisciplinary management of malnutrition in IBD patients are crucial for improving survival and outcomes related to hospitalization for GIB.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Karecia Byfield, MBBS1, Phuuwadith Wattanachayakul, MD1, Nino Gudushauri, MD2, Tinsae Anebo, MD1, Colton F. Jones, MBBS1, Fnu Deepali, MD3, Megan Johnson, MBBS4, Elvis Obomanu, MBBS5, Carlo Gabriel C. Casipit, MD1, Jordan Carty, MD1, Kevin Robinson, MD1, James Walter, MD6. P0927 - Impact of Malnutrition on Outcomes of Patients With Inflammatory Bowel Disease Hospitalized for Gastrointestinal Bleeding: A Propensity Score-Matched Study From a U.S. Collaborative Network, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Albert Einstein Medical Center, Philadelphia, PA; 2Jefferson Einstein Hospital, Philadelphia, PA; 3Einstein Medical Center, Philadelphia, PA; 4Spanish Town Hospital, Kingston, Saint Andrew, Jamaica; 5Jefferson-Einstein Hospital, Philadelphia, PA; 6Einstein Healthcare Network, Philadelphia, PA
Introduction: Recent data highlight the complex interplay between malnutrition and inflammatory bowel disease (IBD), leading to adverse outcomes such as increased disease activity, poor therapy response, and diminished quality of life. However, the impact of malnutrition on patients with Crohn’s disease or ulcerative colitis hospitalized for gastrointestinal bleeding (GIB) remains unclear.
Methods: Data from the US Collaborative Network-TriNetX was used to evaluate the impact of malnutrition on IBD patients hospitalized for GIB. Patients were classified into two cohorts: those with malnutrition and those without as identified by the relevant ICD-10 codes. The malnutrition cohort was propensity score-matched with the control group based on age, sex, race, and comorbidities. Patients were then followed for 30 days post-hospitalization to assess outcomes including mortality, hypovolemic shock, perforation, ICU admission, need for transfusion, and endoscopic procedures.
Results: After propensity score matching, each cohort consisted of 1,614 patients with similar baseline characteristics. The mean age was 55.7 years for the malnutrition group and 54.2 years for the non-malnutrition group. Both cohorts were 46% female. The ethnicity distribution was 68% White, 12% Black, and 6% Hispanic. Within 30 days post-hospitalization, patients with malnutrition had a significantly increased risk of all-cause mortality (RR: 2.7, 95% CI: 1.73-4.34, P< 0.0001), shock (RR: 3.08, 95% CI: 1.50-6.30, P< 0.01), and ICU admission (RR: 2.54, 95% CI: 1.97-3.28, P< 0.001). In addition, heightened risk for endoscopic procedures (RR: 1.5, 95% CI: 1.10-2.04, P< 0.01) and blood transfusions (RR: 1.83, 95% CI: 1.14-2.93, P=0.01) was found in the cohort with malnutrition compared to the cohort without. No significant differences were found in the risk of toxic megacolon, perforation, or readmission.
Discussion: Our study found that malnutrition is a major predictor of adverse short-term outcomes among IBD patients hospitalized for GIB, including higher mortality rates, increased ICU admissions, and a greater need for endoscopic procedures. Prompt identification and multidisciplinary management of malnutrition in IBD patients are crucial for improving survival and outcomes related to hospitalization for GIB.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Karecia Byfield indicated no relevant financial relationships.
Phuuwadith Wattanachayakul indicated no relevant financial relationships.
Nino Gudushauri indicated no relevant financial relationships.
Tinsae Anebo indicated no relevant financial relationships.
Colton Jones indicated no relevant financial relationships.
Fnu Deepali indicated no relevant financial relationships.
Megan Johnson indicated no relevant financial relationships.
Elvis Obomanu indicated no relevant financial relationships.
Carlo Gabriel Casipit indicated no relevant financial relationships.
Jordan Carty indicated no relevant financial relationships.
Kevin Robinson indicated no relevant financial relationships.
James Walter: Eli Lilly – Advisor or Review Panel Member. Medtronic – Consultant.
Karecia Byfield, MBBS1, Phuuwadith Wattanachayakul, MD1, Nino Gudushauri, MD2, Tinsae Anebo, MD1, Colton F. Jones, MBBS1, Fnu Deepali, MD3, Megan Johnson, MBBS4, Elvis Obomanu, MBBS5, Carlo Gabriel C. Casipit, MD1, Jordan Carty, MD1, Kevin Robinson, MD1, James Walter, MD6. P0927 - Impact of Malnutrition on Outcomes of Patients With Inflammatory Bowel Disease Hospitalized for Gastrointestinal Bleeding: A Propensity Score-Matched Study From a U.S. Collaborative Network, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
