Sunday Poster Session
Category: IBD
P0830 - Rectal Cuff Inflammation on Initial Pouchoscopy is Associated with Neoplasia Development in IBD Patients With an Ileal Pouch-Anal Anastomosis: A Case-Control Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Joseph Carter Powers, BA
Cleveland Clinic Lerner College of Medicine
Cleveland, OH
Presenting Author(s)
Joseph Carter Powers, BA1, Mark Zemanek, DO2, Katherine Westbrook Cates, DO3, Emma F. Dester, MS1, Mili Dave, BA4, Tracy Hull, MD5, Olga Lavryk, MD2, Benjamin L. Cohen, MD2, Edward Barnes, MD, MPH, FACG4, Taha Qazi, MD6
1Cleveland Clinic Lerner College of Medicine, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Louisiana State University Health, Cleveland, OH; 4University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 5Cleveland Clinic, Cleveland, OH; 6Cleveland Clinic Foundation, Beachwood, OH
Introduction: Patients with an ileal pouch-anal anastomosis (IPAA) are at risk for neoplasia of the pouch and rectal cuff. There are numerous purported risk factors for neoplasia including chronic cuff inflammation, but there is a lack of research assessing this potential relationship. The objective of this study was to assess if cuff inflammation identified during one’s initial pouchoscopy following surgery is associated with neoplasia development.
Methods: This two-institution case-control study included inflammatory bowel disease (IBD) patients with neoplasia of the rectal cuff or ileal pouch who were age- and sex-matched in a 1:4 ratio to controls without neoplasia. Neoplasia was defined as dysplasia (low/high grade) or cancer (adenocarcinoma). Cuff inflammation was defined as description of erythema, edema, and ulcerations, which was verified by a provider with expertise in inflammatory pouch diseases. A multivariable logistic regression was used to assess for association between initial cuff inflammation and neoplasia while adjusting for potential confounders.
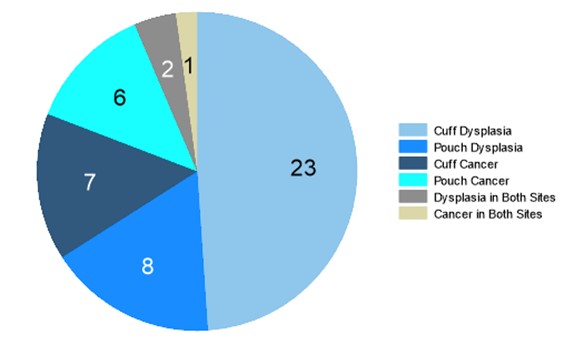
Results: A total of 47 cases of neoplasia were identified and matched to 188 controls. Most patients had a diagnosis of ulcerative colitis (93.2%) with a small number having a diagnosis of Crohn’s disease or indeterminate colitis (3.4% each). Individuals in the case group had a longer interval between final surgery and first pouchoscopy compared to controls (median 2.2 vs. 1.1 years; p < 0.001) and were more likely to demonstrate cuff inflammation on initial pouchoscopy (51% vs. 33%, p = 0.024). Rectal cuff dysplasia was most common (Figure 1; n = 23), followed by pouch dysplasia, cuff cancer, pouch cancer, and neoplasia of both sites. The median time to neoplasia development was 21.6 (IQR 13.3-33.3) years after surgical completion with event times ranging from 0.4-43.4 years. On multivariable analysis, individuals with initial cuff inflammation had a nearly 3 times higher odds of neoplasia (Table 1; aOR = 2.91; 95% CI 1.29-6.57; p = 0.010) while adjusting for follow-up time, primary sclerosing cholangitis (PSC), and surgical indication of neoplasia. A surgical indication of neoplasia was also associated with a higher risk of neoplasia (aOR = 3.86; 95% CI 1.60-9.32; p = 0.003).
Discussion: Initial rectal cuff inflammation is associated with development of rectal cuff and ileal pouch neoplasia in IBD patients with an IPAA. This endoscopic finding should be included with other risk factors when evaluating a patient’s risk for neoplasia.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Joseph Carter Powers, BA1, Mark Zemanek, DO2, Katherine Westbrook Cates, DO3, Emma F. Dester, MS1, Mili Dave, BA4, Tracy Hull, MD5, Olga Lavryk, MD2, Benjamin L. Cohen, MD2, Edward Barnes, MD, MPH, FACG4, Taha Qazi, MD6. P0830 - Rectal Cuff Inflammation on Initial Pouchoscopy is Associated with Neoplasia Development in IBD Patients With an Ileal Pouch-Anal Anastomosis: A Case-Control Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Lerner College of Medicine, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Louisiana State University Health, Cleveland, OH; 4University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 5Cleveland Clinic, Cleveland, OH; 6Cleveland Clinic Foundation, Beachwood, OH
Introduction: Patients with an ileal pouch-anal anastomosis (IPAA) are at risk for neoplasia of the pouch and rectal cuff. There are numerous purported risk factors for neoplasia including chronic cuff inflammation, but there is a lack of research assessing this potential relationship. The objective of this study was to assess if cuff inflammation identified during one’s initial pouchoscopy following surgery is associated with neoplasia development.
Methods: This two-institution case-control study included inflammatory bowel disease (IBD) patients with neoplasia of the rectal cuff or ileal pouch who were age- and sex-matched in a 1:4 ratio to controls without neoplasia. Neoplasia was defined as dysplasia (low/high grade) or cancer (adenocarcinoma). Cuff inflammation was defined as description of erythema, edema, and ulcerations, which was verified by a provider with expertise in inflammatory pouch diseases. A multivariable logistic regression was used to assess for association between initial cuff inflammation and neoplasia while adjusting for potential confounders.
Results: A total of 47 cases of neoplasia were identified and matched to 188 controls. Most patients had a diagnosis of ulcerative colitis (93.2%) with a small number having a diagnosis of Crohn’s disease or indeterminate colitis (3.4% each). Individuals in the case group had a longer interval between final surgery and first pouchoscopy compared to controls (median 2.2 vs. 1.1 years; p < 0.001) and were more likely to demonstrate cuff inflammation on initial pouchoscopy (51% vs. 33%, p = 0.024). Rectal cuff dysplasia was most common (Figure 1; n = 23), followed by pouch dysplasia, cuff cancer, pouch cancer, and neoplasia of both sites. The median time to neoplasia development was 21.6 (IQR 13.3-33.3) years after surgical completion with event times ranging from 0.4-43.4 years. On multivariable analysis, individuals with initial cuff inflammation had a nearly 3 times higher odds of neoplasia (Table 1; aOR = 2.91; 95% CI 1.29-6.57; p = 0.010) while adjusting for follow-up time, primary sclerosing cholangitis (PSC), and surgical indication of neoplasia. A surgical indication of neoplasia was also associated with a higher risk of neoplasia (aOR = 3.86; 95% CI 1.60-9.32; p = 0.003).
Discussion: Initial rectal cuff inflammation is associated with development of rectal cuff and ileal pouch neoplasia in IBD patients with an IPAA. This endoscopic finding should be included with other risk factors when evaluating a patient’s risk for neoplasia.
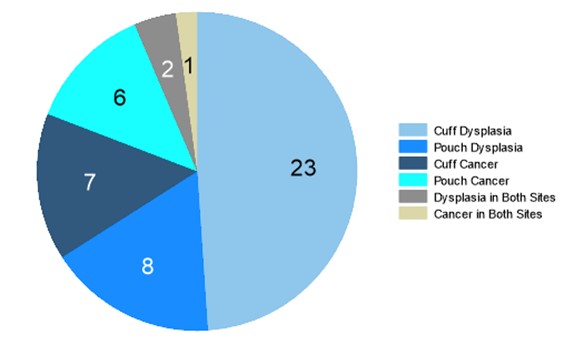
Figure: Figure 1: Graphical Representation of Neoplasia Cases Organized by Type and Site. Numbers presented on each slice correspond to the total number of individuals with neoplasia of that type and site combination.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Joseph Carter Powers: The Crohn's and Colitis Foundation Grant Funding through the Student Research Fellowship Award – Grant/Research Support.
Mark Zemanek indicated no relevant financial relationships.
Katherine Westbrook Cates indicated no relevant financial relationships.
Emma Dester indicated no relevant financial relationships.
Mili Dave indicated no relevant financial relationships.
Tracy Hull indicated no relevant financial relationships.
Olga Lavryk indicated no relevant financial relationships.
Benjamin L. Cohen: Abbvie – Consultant, support and/or funding, Speakers Bureau. Bristol Myers Squibb – support and/or funding. Celgene – support and/or funding. Emmes – Consultant, Speakers Bureau. Janssen – Consultant, support and/or funding, Speakers Bureau. Pfizer – support and/or funding. Takeda – Consultant, Speakers Bureau. Target RWE – Consultant, Speakers Bureau.
Edward Barnes: AbbVie, Inc. – Consultant. Boomerang – Consultant. Bristol-Meyers Squibb – Consultant. Direct Biologics – Consultant. Eli Lilly and Company – Advisor or Review Panel Member. Pfizer – Consultant. Target RWE – Consultant.
Taha Qazi: Abbvie Biosciences – Advisor or Review Panel Member, Consultant, Grant/Research Support, Speakers Bureau. Celgene/BMS – Advisor or Review Panel Member, Speakers Bureau. Janssen – Speakers Bureau. Pfizer – Advisor or Review Panel Member, Advisory Committee/Board Member. Prometheus Biosciences – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant.
Joseph Carter Powers, BA1, Mark Zemanek, DO2, Katherine Westbrook Cates, DO3, Emma F. Dester, MS1, Mili Dave, BA4, Tracy Hull, MD5, Olga Lavryk, MD2, Benjamin L. Cohen, MD2, Edward Barnes, MD, MPH, FACG4, Taha Qazi, MD6. P0830 - Rectal Cuff Inflammation on Initial Pouchoscopy is Associated with Neoplasia Development in IBD Patients With an Ileal Pouch-Anal Anastomosis: A Case-Control Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
