Sunday Poster Session
Category: IBD
P0835 - Outcomes of Isolated Recurrent, Persistent Complex Perianal Fistulas Without Luminal Crohn’s Disease: A Case Series of 24 Patients
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Hannah Fiske, MD
Brown University / Rhode Island Hospital
Providence, RI
Presenting Author(s)
Hannah Fiske, MD1, Chung Sang Tse, MD2, Badr Al-Bawardy, MD3, Pooja Magavi, MD4, Gauree Konijeti, MD, MPH5, Eric Mao, MD6, Sean Fine, MD7, Alyssa Parian, MD8, Mark Lazarev, MD9, Samir Shah, MD10
1Brown University / Rhode Island Hospital, Providence, RI; 2University of Pennsylvania, Philadelphia, PA; 3King Faisal Specialist Hospital and Research Centre, Riyadh, Ar Riyad, Saudi Arabia; 4Scripps Clinic, San Diego, CA; 5Scripps Clinic, La Jolla, CA; 6University of California, Davis, Sacramento, CA; 7Brown Medicine/Lifespan, Providence, RI; 8The Johns Hopkins Hospital, Baltimore, MD; 9Johns Hopkins University School of Medicine, Baltimore, MD; 10Gastroenterology Associates, Providence, RI
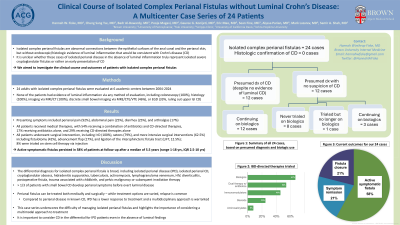
Introduction: Isolated complex perianal fistulas, without luminal evidence of Crohn’s disease (CD), pose diagnostic and treatment dilemmas for gastroenterologists and colorectal surgeons. For patients who develop recurrent complex fistulas, a presumptive diagnosis of CD is often made. It is unclear whether these cases of isolated perianal disease, in the absence of luminal inflammation, represent truly isolated severe cryptoglandular fistulas or rather an early presentation of undiagnosed CD. This renders the best management approach a clinical challenge.
Methods: Data was collected retrospectively from 6 academic medical centers on 24 adults who presented with isolated complex perianal fistulas. Initial presenting symptoms, diagnostic evaluations, medical and surgical treatments pursued, and ultimate diagnosis/outcome and plan for each patient were compiled.
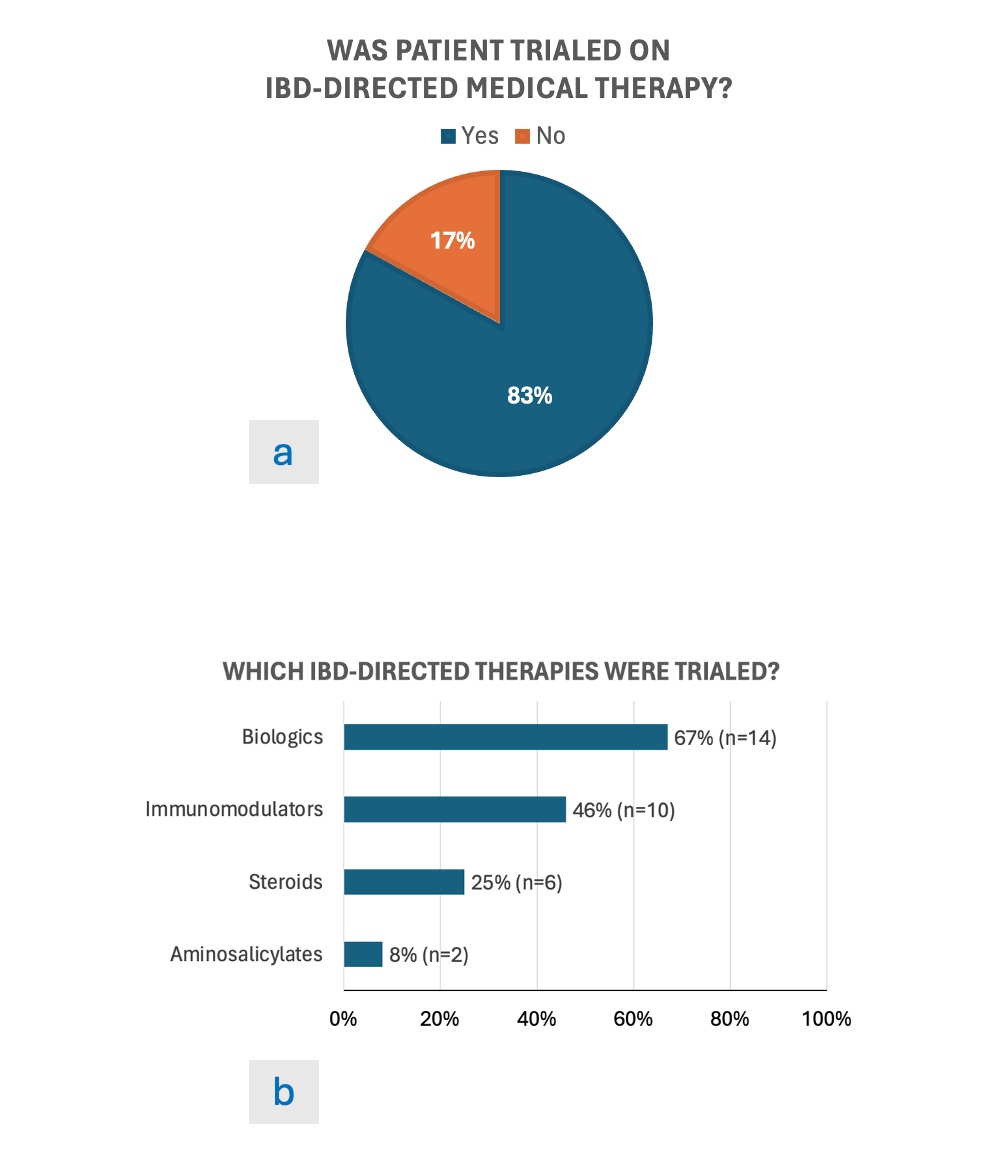
Results: 24 patients were included in this study (15 women, 9 men; mean age 33 years). Presenting symptoms included perianal pain (92%), abdominal pain (25%), diarrhea (25%), and arthralgia (17%). All patients underwent colonoscopy without evidence of inflammation on endoscopy or histology. Further workup including computed tomography, magnetic resonance imaging, video capsule endoscopy, computed tomography elastography, and magnetic resonance elastography did not reveal luminal inflammation. Medical management included antibiotics (71%) and IBD-directed therapies (83%; with 67% receiving biologics). Surgical therapies were pursued in all patients, including exam under anesthesia with incision and drainage (100%), setons (79%), and fistulotomy (42%). Despite surgical and medical management, active symptomatic complex perianal fistulas persisted in 58% of patients at follow-up after median 5.5 years (IQR 2.5-10 years).
Discussion: The cases described in our cohort reveal the importance of a multimodal approach when treating isolated perianal disease in the absence of luminal CD. Isolated perianal disease is classically treated with antibiotics and local surgical intervention, whereas perianal CD treatment is more complex, incorporating the use of immunomodulatory therapy, particularly anti-tumor necrosis factor agents with thiopurines. Compared to perianal disease in known CD, isolated perianal disease has a lower response to treatment and a multidisciplinary approach is warranted. This case series provides insight for clinicians on treatment possibilities and outcomes with isolated perianal disease.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Hannah Fiske, MD1, Chung Sang Tse, MD2, Badr Al-Bawardy, MD3, Pooja Magavi, MD4, Gauree Konijeti, MD, MPH5, Eric Mao, MD6, Sean Fine, MD7, Alyssa Parian, MD8, Mark Lazarev, MD9, Samir Shah, MD10. P0835 - Outcomes of Isolated Recurrent, Persistent Complex Perianal Fistulas Without Luminal Crohn’s Disease: A Case Series of 24 Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brown University / Rhode Island Hospital, Providence, RI; 2University of Pennsylvania, Philadelphia, PA; 3King Faisal Specialist Hospital and Research Centre, Riyadh, Ar Riyad, Saudi Arabia; 4Scripps Clinic, San Diego, CA; 5Scripps Clinic, La Jolla, CA; 6University of California, Davis, Sacramento, CA; 7Brown Medicine/Lifespan, Providence, RI; 8The Johns Hopkins Hospital, Baltimore, MD; 9Johns Hopkins University School of Medicine, Baltimore, MD; 10Gastroenterology Associates, Providence, RI
Introduction: Isolated complex perianal fistulas, without luminal evidence of Crohn’s disease (CD), pose diagnostic and treatment dilemmas for gastroenterologists and colorectal surgeons. For patients who develop recurrent complex fistulas, a presumptive diagnosis of CD is often made. It is unclear whether these cases of isolated perianal disease, in the absence of luminal inflammation, represent truly isolated severe cryptoglandular fistulas or rather an early presentation of undiagnosed CD. This renders the best management approach a clinical challenge.
Methods: Data was collected retrospectively from 6 academic medical centers on 24 adults who presented with isolated complex perianal fistulas. Initial presenting symptoms, diagnostic evaluations, medical and surgical treatments pursued, and ultimate diagnosis/outcome and plan for each patient were compiled.
Results: 24 patients were included in this study (15 women, 9 men; mean age 33 years). Presenting symptoms included perianal pain (92%), abdominal pain (25%), diarrhea (25%), and arthralgia (17%). All patients underwent colonoscopy without evidence of inflammation on endoscopy or histology. Further workup including computed tomography, magnetic resonance imaging, video capsule endoscopy, computed tomography elastography, and magnetic resonance elastography did not reveal luminal inflammation. Medical management included antibiotics (71%) and IBD-directed therapies (83%; with 67% receiving biologics). Surgical therapies were pursued in all patients, including exam under anesthesia with incision and drainage (100%), setons (79%), and fistulotomy (42%). Despite surgical and medical management, active symptomatic complex perianal fistulas persisted in 58% of patients at follow-up after median 5.5 years (IQR 2.5-10 years).
Discussion: The cases described in our cohort reveal the importance of a multimodal approach when treating isolated perianal disease in the absence of luminal CD. Isolated perianal disease is classically treated with antibiotics and local surgical intervention, whereas perianal CD treatment is more complex, incorporating the use of immunomodulatory therapy, particularly anti-tumor necrosis factor agents with thiopurines. Compared to perianal disease in known CD, isolated perianal disease has a lower response to treatment and a multidisciplinary approach is warranted. This case series provides insight for clinicians on treatment possibilities and outcomes with isolated perianal disease.
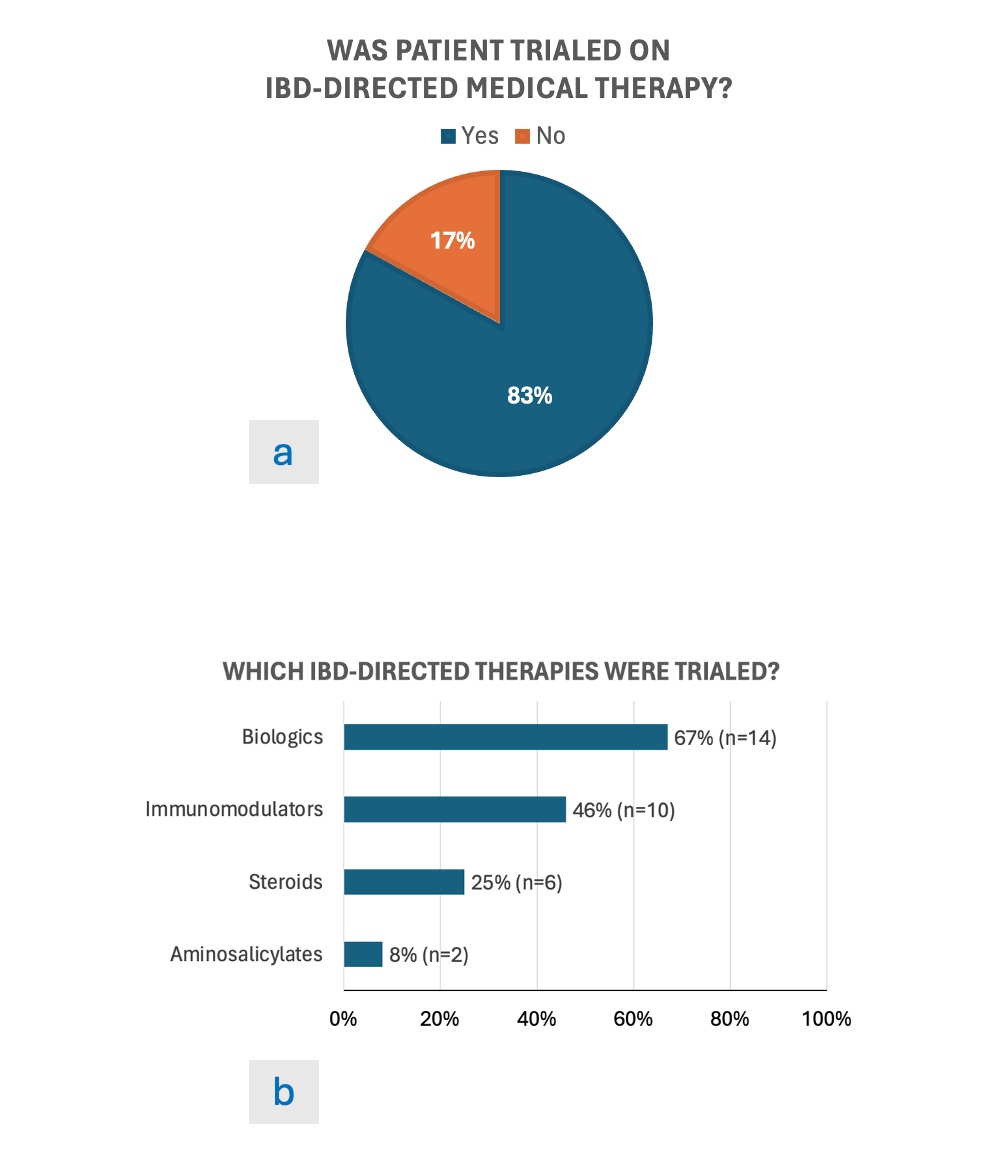
Figure: Image 1
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Hannah Fiske indicated no relevant financial relationships.
Chung Sang Tse indicated no relevant financial relationships.
Badr Al-Bawardy: AbbVie – Consultant, Speakers Bureau. Janssen – Speakers Bureau. Pfizer – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Takeda – Speakers Bureau.
Pooja Magavi indicated no relevant financial relationships.
Gauree Konijeti: Abbvie – Advisory Committee/Board Member, Consultant. Lilly – Consultant, Speakers Bureau. Pfizer – Advisory Committee/Board Member. Takeda – Speakers Bureau.
Eric Mao indicated no relevant financial relationships.
Sean Fine: Abbvie – Advisory Committee/Board Member. Bristol Myers Squibb – Consultant. Takeda – Advisory Committee/Board Member.
Alyssa Parian indicated no relevant financial relationships.
Mark Lazarev: Johnson and Johnson – Advisory Committee/Board Member.
Samir Shah: Roche Information Systems – Consultant.
Hannah Fiske, MD1, Chung Sang Tse, MD2, Badr Al-Bawardy, MD3, Pooja Magavi, MD4, Gauree Konijeti, MD, MPH5, Eric Mao, MD6, Sean Fine, MD7, Alyssa Parian, MD8, Mark Lazarev, MD9, Samir Shah, MD10. P0835 - Outcomes of Isolated Recurrent, Persistent Complex Perianal Fistulas Without Luminal Crohn’s Disease: A Case Series of 24 Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
