Sunday Poster Session
Category: IBD
P0839 - Comparing Rates of Periodontitis in IBS and IBD Patients: A Multi-Network Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- JH
Jacques Halabi, MD
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Jacques Halabi, MD1, Jenny Jan, MD2, Jaime A. Perez, PhD3, Preetika Sinh, MD4, Gregory Cooper, MD5, Vu Q. Nguyen, MD, MS5, Jeffry Katz, MD5, Fabio Cominelli, MD, PhD5, Miguel D Regueiro, MD6, Emad Mansoor, MD5
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Cleveland, OH; 3University Hospitals Clinical Research Center, Cleveland, OH; 4Medical College of Wisconsin, Milwaukee, WI; 5Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 6Cleveland Clinic, Cleveland, OH
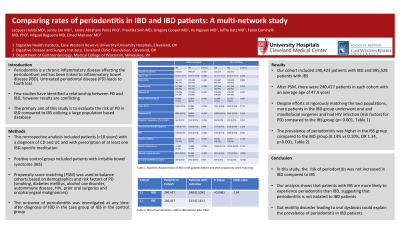
Introduction: Periodontitis is a chronic inflammatory disease that affects the periodontium and has been linked to inflammatory bowel disease (IBD). Untreated periodontal disease (PD) can lead to tooth loss. A limited number of studies have identified a relationship between PD and IBD through the “oral-gut axis”, however results are conflicting. In addition, most control groups in these studies consisted of healthy patients. We sought to evaluate the risk of PD in IBD (a chronic inflammatory disorder) compared to IBS (a functional GI disorder) utilizing a large population based database.
Methods: Using TriNetX, a de-identified database collecting real-time data on over 113 million patients, we performed a retrospective study identifying all adults (aged >18 years) with a diagnosis of CD and UC and with prescription of at least one IBD-specific medication. Positive control group included patients with irritable bowel syndrome (IBS). We used propensity score matching (PSM) to balance cohorts based on demographics, and risk factors of PD ( smoking, diabetes mellitus, alcohol use disorder, autoimmune disease, HIV, prior oral surgeries and oropharyngeal malignancies). We investigated the outcome of periodontitis at any time after diagnosis of IBD in the case group or IBS in the control group. We calculated baseline difference using independent t-tests and chi-square tests. Odds ratios and 95% confidence intervals were reported and P-values < 0.05 were considered statistically significant.
Results: Our cohort included 240,423 patients with IBD and 995,528 patients with IBS. After PSM, there were 240,417 patients in each cohort with an average age of 47.4 years. Despite efforts at rigorously matching the two populations, more patients in the IBD group underwent oral and maxillofacial surgeries and had HIV infection (risk factors for PD) compared to the IBS group ( p< 0.001, Table 1). However the prevalence of periodontitis was higher in the IBS group compared to the IBD group (0.14% vs 0.10%, OR 1.34, p=0.001, Table 1).
Discussion: The mechanism linking IBD and periodontitis appears to be driven by common altered immune inflammatory mechanisms. In this study, we did not find an increased risk of periodontitis in IBD compared to IBS. Our analysis shows that patients with IBS are more likely to experience periodontitis than IBD, suggesting that periodontitis is not isolated to patients with IBD. Gut motility disorder leading to oral dysbiosis could explain the prevalence of periodontitis in IBS patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jacques Halabi, MD1, Jenny Jan, MD2, Jaime A. Perez, PhD3, Preetika Sinh, MD4, Gregory Cooper, MD5, Vu Q. Nguyen, MD, MS5, Jeffry Katz, MD5, Fabio Cominelli, MD, PhD5, Miguel D Regueiro, MD6, Emad Mansoor, MD5. P0839 - Comparing Rates of Periodontitis in IBS and IBD Patients: A Multi-Network Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Cleveland, OH; 3University Hospitals Clinical Research Center, Cleveland, OH; 4Medical College of Wisconsin, Milwaukee, WI; 5Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 6Cleveland Clinic, Cleveland, OH
Introduction: Periodontitis is a chronic inflammatory disease that affects the periodontium and has been linked to inflammatory bowel disease (IBD). Untreated periodontal disease (PD) can lead to tooth loss. A limited number of studies have identified a relationship between PD and IBD through the “oral-gut axis”, however results are conflicting. In addition, most control groups in these studies consisted of healthy patients. We sought to evaluate the risk of PD in IBD (a chronic inflammatory disorder) compared to IBS (a functional GI disorder) utilizing a large population based database.
Methods: Using TriNetX, a de-identified database collecting real-time data on over 113 million patients, we performed a retrospective study identifying all adults (aged >18 years) with a diagnosis of CD and UC and with prescription of at least one IBD-specific medication. Positive control group included patients with irritable bowel syndrome (IBS). We used propensity score matching (PSM) to balance cohorts based on demographics, and risk factors of PD ( smoking, diabetes mellitus, alcohol use disorder, autoimmune disease, HIV, prior oral surgeries and oropharyngeal malignancies). We investigated the outcome of periodontitis at any time after diagnosis of IBD in the case group or IBS in the control group. We calculated baseline difference using independent t-tests and chi-square tests. Odds ratios and 95% confidence intervals were reported and P-values < 0.05 were considered statistically significant.
Results: Our cohort included 240,423 patients with IBD and 995,528 patients with IBS. After PSM, there were 240,417 patients in each cohort with an average age of 47.4 years. Despite efforts at rigorously matching the two populations, more patients in the IBD group underwent oral and maxillofacial surgeries and had HIV infection (risk factors for PD) compared to the IBS group ( p< 0.001, Table 1). However the prevalence of periodontitis was higher in the IBS group compared to the IBD group (0.14% vs 0.10%, OR 1.34, p=0.001, Table 1).
Discussion: The mechanism linking IBD and periodontitis appears to be driven by common altered immune inflammatory mechanisms. In this study, we did not find an increased risk of periodontitis in IBD compared to IBS. Our analysis shows that patients with IBS are more likely to experience periodontitis than IBD, suggesting that periodontitis is not isolated to patients with IBD. Gut motility disorder leading to oral dysbiosis could explain the prevalence of periodontitis in IBS patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jacques Halabi indicated no relevant financial relationships.
Jenny Jan indicated no relevant financial relationships.
Jaime Perez indicated no relevant financial relationships.
Preetika Sinh: Bristol Myers Squibb – Advisory Committee/Board Member.
Gregory Cooper indicated no relevant financial relationships.
Vu Nguyen: AbbVie – Speakers Bureau. Eli Lilly – Speakers Bureau.
Jeffry Katz indicated no relevant financial relationships.
Fabio Cominelli indicated no relevant financial relationships.
Miguel D Regueiro: AbbVie – Advisory Committee/Board Member, Consultant, Speakers Bureau.
Emad Mansoor: Lilly – Speakers Bureau. Takeda – Speakers Bureau.
Jacques Halabi, MD1, Jenny Jan, MD2, Jaime A. Perez, PhD3, Preetika Sinh, MD4, Gregory Cooper, MD5, Vu Q. Nguyen, MD, MS5, Jeffry Katz, MD5, Fabio Cominelli, MD, PhD5, Miguel D Regueiro, MD6, Emad Mansoor, MD5. P0839 - Comparing Rates of Periodontitis in IBS and IBD Patients: A Multi-Network Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
