Sunday Poster Session
Category: IBD
P0842 - Inflammatory Bowel Disease is Associated With Increased Risk of Cardiovascular Events but Not Mortality. Data From a Large U.S. National Database
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- SB
Saffia Bajwa, DO
Medical College of Wisconsin
Wauwatosa, WI
Presenting Author(s)
Saffia Bajwa, DO1, Paraj Patel, MD1, Omair Iqbal, BS1, Divyanshu Mohananey, MD1, Masoud Khani, MD2, Jake Lou, PhD3, Daniel J.. Stein, MD4, Jana G. Hashash, MD, MSc5, Emad Mansoor, MD6, Raymond K. Cross, MD, MS, FACG7, Preetika Sinh, MD4
1Medical College of Wisconsin, Wauwatosa, WI; 2University of Wisconsin, Madison, WI; 3Medical College of Wisconsin, Madison, WI; 4Medical College of Wisconsin, Milwaukee, WI; 5Mayo Clinic, Jacksonville, FL; 6Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 7Melissa L. Posner Institute for Digestive Health & Liver Disease at Mercy Medical Center, Baltimore, MD
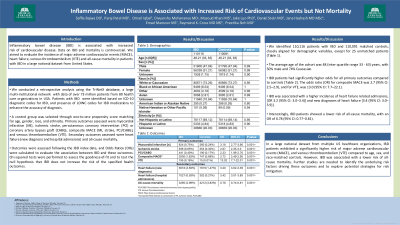
Introduction: Inflammatory bowel disease (IBD) is associated with increased risk of cardiovascular disease. Data on IBD and mortality is controversial. We aimed to evaluate the incidence of major adverse cardiovascular events (MACE), heart failure, venous thromboembolism (VTE) and all-cause mortality in IBD patients in a large national dataset from United States.
Methods: We performed retrospective analysis using a large multi-institutional database, TriNetX. IBD patients were identified using ICD10 codes for IBD and presence of LONIC codes for IBD medications (to increase the validity of diagnosis codes). A control group was selected and matched one-to-one for age, gender, race, and ethnicity to assess primary (myocardial infarction (MI), ischemic stroke, percutaneous coronary intervention (PCI)/coronary artery bypass graft (CABG), composite MACE (MI, stroke, PCI/CABG), VTE) and secondary outcomes (heart failure: new diagnosis and hospital admissions), and all-cause mortality. Outcomes were assessed after the IBD index date. Odds Ratios (ORs) were used as a measure to assess association between IBD and outcomes. Additionally, the Chi-squared test was applied to assess the goodness-of-fit and to test the null hypothesis that IBD does not increase the risk of specified health outcomes.
Results: We identified 110,116 IBD and 110091 controls (closely matched for demographic variables with matching not possible for 25 patients). Average age of the cohort was 48 years with 50% being male and 74% Caucasian. Results show significantly higher OR for all primary outcomes in IBD patients [composite MACE: OR 2.7, 95% CI 2.5 - 2.9, VTE: OR 13 ,95% CI 7.7 -22.1] (Table). IBD was also associated with higher incidence of heart failure [new diagnosis OR 3.2, 95% CI 3.0 – 3.4, hospital admissions OR 3.4, 95% CI 3.0-3.9). However, IBD patients had lower risk of all-cause mortality [OR of 0.78, 95% CI 0.77- 0.81].
Discussion: In a large national dataset from multiple US health care organizations, IBD patients have a higher risk of MACE and VTE as compared to their age, sex and race matched controls suggesting that the disease could be driving the higher risk of cardiovascular events. IBD, was however, associated with lower risk of all-cause mortality. Further studies are needed to assess the risk factors effecting these outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Saffia Bajwa, DO1, Paraj Patel, MD1, Omair Iqbal, BS1, Divyanshu Mohananey, MD1, Masoud Khani, MD2, Jake Lou, PhD3, Daniel J.. Stein, MD4, Jana G. Hashash, MD, MSc5, Emad Mansoor, MD6, Raymond K. Cross, MD, MS, FACG7, Preetika Sinh, MD4. P0842 - Inflammatory Bowel Disease is Associated With Increased Risk of Cardiovascular Events but Not Mortality. Data From a Large U.S. National Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Medical College of Wisconsin, Wauwatosa, WI; 2University of Wisconsin, Madison, WI; 3Medical College of Wisconsin, Madison, WI; 4Medical College of Wisconsin, Milwaukee, WI; 5Mayo Clinic, Jacksonville, FL; 6Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 7Melissa L. Posner Institute for Digestive Health & Liver Disease at Mercy Medical Center, Baltimore, MD
Introduction: Inflammatory bowel disease (IBD) is associated with increased risk of cardiovascular disease. Data on IBD and mortality is controversial. We aimed to evaluate the incidence of major adverse cardiovascular events (MACE), heart failure, venous thromboembolism (VTE) and all-cause mortality in IBD patients in a large national dataset from United States.
Methods: We performed retrospective analysis using a large multi-institutional database, TriNetX. IBD patients were identified using ICD10 codes for IBD and presence of LONIC codes for IBD medications (to increase the validity of diagnosis codes). A control group was selected and matched one-to-one for age, gender, race, and ethnicity to assess primary (myocardial infarction (MI), ischemic stroke, percutaneous coronary intervention (PCI)/coronary artery bypass graft (CABG), composite MACE (MI, stroke, PCI/CABG), VTE) and secondary outcomes (heart failure: new diagnosis and hospital admissions), and all-cause mortality. Outcomes were assessed after the IBD index date. Odds Ratios (ORs) were used as a measure to assess association between IBD and outcomes. Additionally, the Chi-squared test was applied to assess the goodness-of-fit and to test the null hypothesis that IBD does not increase the risk of specified health outcomes.
Results: We identified 110,116 IBD and 110091 controls (closely matched for demographic variables with matching not possible for 25 patients). Average age of the cohort was 48 years with 50% being male and 74% Caucasian. Results show significantly higher OR for all primary outcomes in IBD patients [composite MACE: OR 2.7, 95% CI 2.5 - 2.9, VTE: OR 13 ,95% CI 7.7 -22.1] (Table). IBD was also associated with higher incidence of heart failure [new diagnosis OR 3.2, 95% CI 3.0 – 3.4, hospital admissions OR 3.4, 95% CI 3.0-3.9). However, IBD patients had lower risk of all-cause mortality [OR of 0.78, 95% CI 0.77- 0.81].
Discussion: In a large national dataset from multiple US health care organizations, IBD patients have a higher risk of MACE and VTE as compared to their age, sex and race matched controls suggesting that the disease could be driving the higher risk of cardiovascular events. IBD, was however, associated with lower risk of all-cause mortality. Further studies are needed to assess the risk factors effecting these outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Saffia Bajwa indicated no relevant financial relationships.
Paraj Patel indicated no relevant financial relationships.
Omair Iqbal indicated no relevant financial relationships.
Divyanshu Mohananey indicated no relevant financial relationships.
Masoud Khani indicated no relevant financial relationships.
Jake Lou indicated no relevant financial relationships.
Daniel Stein: Abbvie – Consultant, Speakers Bureau. BMS – Consultant, Speakers Bureau. Janssen – Speakers Bureau. Lilly – Speakers Bureau. Pfizer – Speakers Bureau. Takeda – Speakers Bureau.
Jana Hashash: Bristol Myers Squibb – Consultant.
Emad Mansoor: Lilly – Speakers Bureau. Takeda – Speakers Bureau.
Raymond K. Cross: AbbVie – Consultant. Adiso – Consultant. Bristol Myers Squibb – Consultant. CorEvitas Registry – scientific co-director. Fresenius Kabi – Consultant. Fzata – Consultant. IBD Education Group – executive committee member. Janssen – Consultant, Grant/Research Support. Magellan Health – Consultant. Option Care Health – Consultant. Pfizer – Consultant. Pharmacosmos – Consultant. Samsung Bioepis – Consultant. Sandoz – Consultant. Sebela – Consultant. Takeda – Consultant.
Preetika Sinh: Bristol Myers Squibb – Advisory Committee/Board Member.
Saffia Bajwa, DO1, Paraj Patel, MD1, Omair Iqbal, BS1, Divyanshu Mohananey, MD1, Masoud Khani, MD2, Jake Lou, PhD3, Daniel J.. Stein, MD4, Jana G. Hashash, MD, MSc5, Emad Mansoor, MD6, Raymond K. Cross, MD, MS, FACG7, Preetika Sinh, MD4. P0842 - Inflammatory Bowel Disease is Associated With Increased Risk of Cardiovascular Events but Not Mortality. Data From a Large U.S. National Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
