Sunday Poster Session
Category: GI Bleeding
P0749 - Do Not Resuscitate Status in Patients With Non-Variceal Upper Gastrointestinal Bleeding: Insights From National Inpatient Sample Database
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

Has Audio

Mhd Kutaiba Albuni, MD
Department of Internal Medicine, TriHealth Inc., Cincinnati
Cincinnati, OH
Presenting Author(s)
Mhd Kutaiba Albuni, MD1, Bisher Sawaf, MD2, Bana Sabbagh, MD3, Fernando R. Mateo, MD3, M Kenan Rahima, MD4, Muddana Venkata, MD3
1TriHealth, Doha, Ad Dawhah, Qatar; 2University of Toledo, Toledo, OH; 3TriHealth, Cincinnati, OH; 4TriHealth Good Samaritan Hospital, Cincinnati, OH
Introduction: Healthcare disparities have been an issue. Recent discussions have focused on health disparities in patients with Do-Not-Resucitate status(DNR) and non-variceal upper gastrointestinal bleeding (NVUGIB), particularly how DNR affects care for the gastrointestinal (GI) system. Limited scientific evidence examines outcomes among patients presenting with NVUGIB and DNR. Thus, our objective was to assess clinical outcomes in this specific population.
Methods: We accessed the National Inpatient Sample 2020 to identify adult patients hospitalized due to NVUGIB who have a code status of DNR. The primary endpoint was inpatient mortality, with secondary endpoints including insurance, racial, and gender disparities. We utilized multivariable logistic regression analysis to estimate clinical outcomes with a significance threshold of P < 0.05.
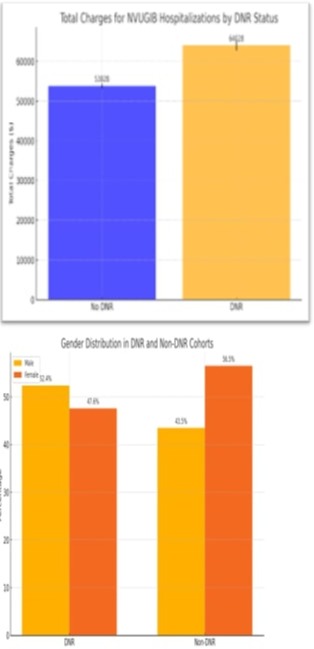
Results: The analysis of hospitalizations for non-variceal upper gastrointestinal bleeding (NVUGIB) and their association with do-not-resuscitate (DNR) status reveals several key findings: The mean age of patients with DNR status (79 years) was notably higher than those without DNR status (66 years), suggesting a higher prevalence of DNR status among older individuals. Males constituted a higher proportion of the DNR cohort (52.4%) compared to the non-DNR cohort (43.5%), indicating potential gender differences in DNR status decision-making. White ethnicity was more prevalent in the DNR cohort (78.9%) compared to the non-DNR cohort (67.08%), suggesting possible racial disparities in DNR status.
In-hospital mortality rates were significantly higher among patients with DNR status (11%) compared to those without DNR status (1.6%), with a substantial odds ratio of 6.8 (95% CI: 6.4-7.0). Female gender was associated with significantly lower odds of death compared to male gender. Racial disparities in mortality odds were observed, with Black, Hispanic, and Native American patients having higher odds of death compared to other racial groups. Higher-income quartiles were associated with lower mortality odds.
Discussion:
The study highlights significant factors influencing mortality, with females and individuals in higher income quartiles showing lower odds of death, while specific racial groups and patients in teaching hospitals exhibit higher odds. These findings indicate the need for targeted healthcare policies and interventions to address these disparities and improve patient outcomes across different demographic and socio-economic groups.
Disclosures:
Mhd Kutaiba Albuni, MD1, Bisher Sawaf, MD2, Bana Sabbagh, MD3, Fernando R. Mateo, MD3, M Kenan Rahima, MD4, Muddana Venkata, MD3. P0749 - Do Not Resuscitate Status in Patients With Non-Variceal Upper Gastrointestinal Bleeding: Insights From National Inpatient Sample Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1TriHealth, Doha, Ad Dawhah, Qatar; 2University of Toledo, Toledo, OH; 3TriHealth, Cincinnati, OH; 4TriHealth Good Samaritan Hospital, Cincinnati, OH
Introduction: Healthcare disparities have been an issue. Recent discussions have focused on health disparities in patients with Do-Not-Resucitate status(DNR) and non-variceal upper gastrointestinal bleeding (NVUGIB), particularly how DNR affects care for the gastrointestinal (GI) system. Limited scientific evidence examines outcomes among patients presenting with NVUGIB and DNR. Thus, our objective was to assess clinical outcomes in this specific population.
Methods: We accessed the National Inpatient Sample 2020 to identify adult patients hospitalized due to NVUGIB who have a code status of DNR. The primary endpoint was inpatient mortality, with secondary endpoints including insurance, racial, and gender disparities. We utilized multivariable logistic regression analysis to estimate clinical outcomes with a significance threshold of P < 0.05.
Results: The analysis of hospitalizations for non-variceal upper gastrointestinal bleeding (NVUGIB) and their association with do-not-resuscitate (DNR) status reveals several key findings: The mean age of patients with DNR status (79 years) was notably higher than those without DNR status (66 years), suggesting a higher prevalence of DNR status among older individuals. Males constituted a higher proportion of the DNR cohort (52.4%) compared to the non-DNR cohort (43.5%), indicating potential gender differences in DNR status decision-making. White ethnicity was more prevalent in the DNR cohort (78.9%) compared to the non-DNR cohort (67.08%), suggesting possible racial disparities in DNR status.
In-hospital mortality rates were significantly higher among patients with DNR status (11%) compared to those without DNR status (1.6%), with a substantial odds ratio of 6.8 (95% CI: 6.4-7.0). Female gender was associated with significantly lower odds of death compared to male gender. Racial disparities in mortality odds were observed, with Black, Hispanic, and Native American patients having higher odds of death compared to other racial groups. Higher-income quartiles were associated with lower mortality odds.
Discussion:
The study highlights significant factors influencing mortality, with females and individuals in higher income quartiles showing lower odds of death, while specific racial groups and patients in teaching hospitals exhibit higher odds. These findings indicate the need for targeted healthcare policies and interventions to address these disparities and improve patient outcomes across different demographic and socio-economic groups.
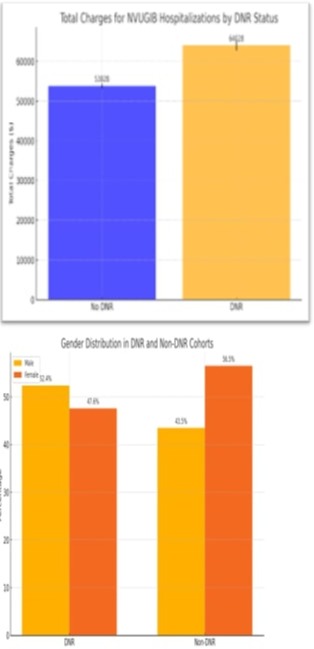
Figure: Total Hospitalization charges and gender disparities between DNR and non-DNR status in patients with NVUGIB
Disclosures:
Mhd Kutaiba Albuni indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Bana Sabbagh indicated no relevant financial relationships.
Fernando Mateo indicated no relevant financial relationships.
M Kenan Rahima indicated no relevant financial relationships.
Muddana Venkata indicated no relevant financial relationships.
Mhd Kutaiba Albuni, MD1, Bisher Sawaf, MD2, Bana Sabbagh, MD3, Fernando R. Mateo, MD3, M Kenan Rahima, MD4, Muddana Venkata, MD3. P0749 - Do Not Resuscitate Status in Patients With Non-Variceal Upper Gastrointestinal Bleeding: Insights From National Inpatient Sample Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
