Sunday Poster Session
Category: GI Bleeding
P0752 - Reducing Use of Inpatient FOBT at an Academic Tertiary Medical Center: A Quality Improvement Project
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Neelima Gaddipati, MD, MBA
Jackson Health System/University of Miami
Miami, FL
Presenting Author(s)
Neelima Gaddipati, MD, MBA1, Sirisha Gaddipati, MD2, Hua Li, MS, MD, PhD3, Ami Panara Shukla, MD2
1Jackson Health System/University of Miami, Miami, FL; 2University of Miami Miller School of Medicine at Jackson Memorial Hospital, Miami, FL; 3University of Miami Health System, Miami, FL
Introduction: The aberrant use of guaiac based fecal occult blood tests (FOBT) persists in inpatient and emergency room settings for diagnosis of gastrointestinal (GI) bleed and/or work up of anemia. Prior studies suggest that inpatient FOBT can increase utilization of hospital resources without providing additional clinical benefit. Our quality improvement project aimed to assess the burden of inpatient FOBT and assess hospital resource utilization after FOBT.
Methods: Using CPT codes, we identified inpatients with FOBT ordered at a single academic hospital from 1/1/2021 to 1/1/2022. We reviewed patient and provider characteristics, overt GI bleed episodes, anemia (hemoglobin preceding FOBT orders), and follow-up care (including GI consult and endoscopies). Associations between diagnoses, GI consults, inpatient endoscopy, and length of stay were analyzed using Pearson’s chi-square, ANOVA, and Wilcoxon rank-sum test using SPSS 29 (IBM, USA).
Results: FOBT was ordered in 247 patients (median age 68 years, 55.1% female). Physicians ordered 64.0% of tests and providers in medicine and its subspecialties ordered 71.3%. Seventy-three (29.5%) had overt GI bleed prior to FOBT. FOBT was negative in 132 instances (53.4%), and in this group there were 37 GI consults (15.0%) and 16 inpatient endoscopies (6.5%). Notably, there were 11 instances where GI was not consulted in a patient with negative FOBT despite report of overt GI bleed. In the 61 patients who underwent endoscopy after FOBT, 65.6% had acute causes of non-hemorrhoidal bleed (see Table 1).
Discussion: Most FOBT were ordered by medicine providers and almost a third were ordered despite overt GI bleed. Although patients with a positive FOBT were more likely to receive a GI consult, 28% with negative FOBT still had a GI consult, suggesting FOBT was not reliable in deciding the next step and as seen in our process map in Figure 1, may have delayed care. In those that underwent endoscopy, we found no difference in the number of patients with acute cause of bleeding between those in the positive and negative groups (p = 0. 127). GI was not consulted in 11 patients that had overt bleed and a negative FOBT, suggesting some providers may be incorrectly relying on FOBT rather than the full clinical picture. We are currently working with hospital stakeholders to create an educational intervention to review diagnostic evaluation of inpatient GI bleeding. Future plans include restricting and eventually removing the test from the inpatient lab orders.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Neelima Gaddipati, MD, MBA1, Sirisha Gaddipati, MD2, Hua Li, MS, MD, PhD3, Ami Panara Shukla, MD2. P0752 - Reducing Use of Inpatient FOBT at an Academic Tertiary Medical Center: A Quality Improvement Project, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Jackson Health System/University of Miami, Miami, FL; 2University of Miami Miller School of Medicine at Jackson Memorial Hospital, Miami, FL; 3University of Miami Health System, Miami, FL
Introduction: The aberrant use of guaiac based fecal occult blood tests (FOBT) persists in inpatient and emergency room settings for diagnosis of gastrointestinal (GI) bleed and/or work up of anemia. Prior studies suggest that inpatient FOBT can increase utilization of hospital resources without providing additional clinical benefit. Our quality improvement project aimed to assess the burden of inpatient FOBT and assess hospital resource utilization after FOBT.
Methods: Using CPT codes, we identified inpatients with FOBT ordered at a single academic hospital from 1/1/2021 to 1/1/2022. We reviewed patient and provider characteristics, overt GI bleed episodes, anemia (hemoglobin preceding FOBT orders), and follow-up care (including GI consult and endoscopies). Associations between diagnoses, GI consults, inpatient endoscopy, and length of stay were analyzed using Pearson’s chi-square, ANOVA, and Wilcoxon rank-sum test using SPSS 29 (IBM, USA).
Results: FOBT was ordered in 247 patients (median age 68 years, 55.1% female). Physicians ordered 64.0% of tests and providers in medicine and its subspecialties ordered 71.3%. Seventy-three (29.5%) had overt GI bleed prior to FOBT. FOBT was negative in 132 instances (53.4%), and in this group there were 37 GI consults (15.0%) and 16 inpatient endoscopies (6.5%). Notably, there were 11 instances where GI was not consulted in a patient with negative FOBT despite report of overt GI bleed. In the 61 patients who underwent endoscopy after FOBT, 65.6% had acute causes of non-hemorrhoidal bleed (see Table 1).
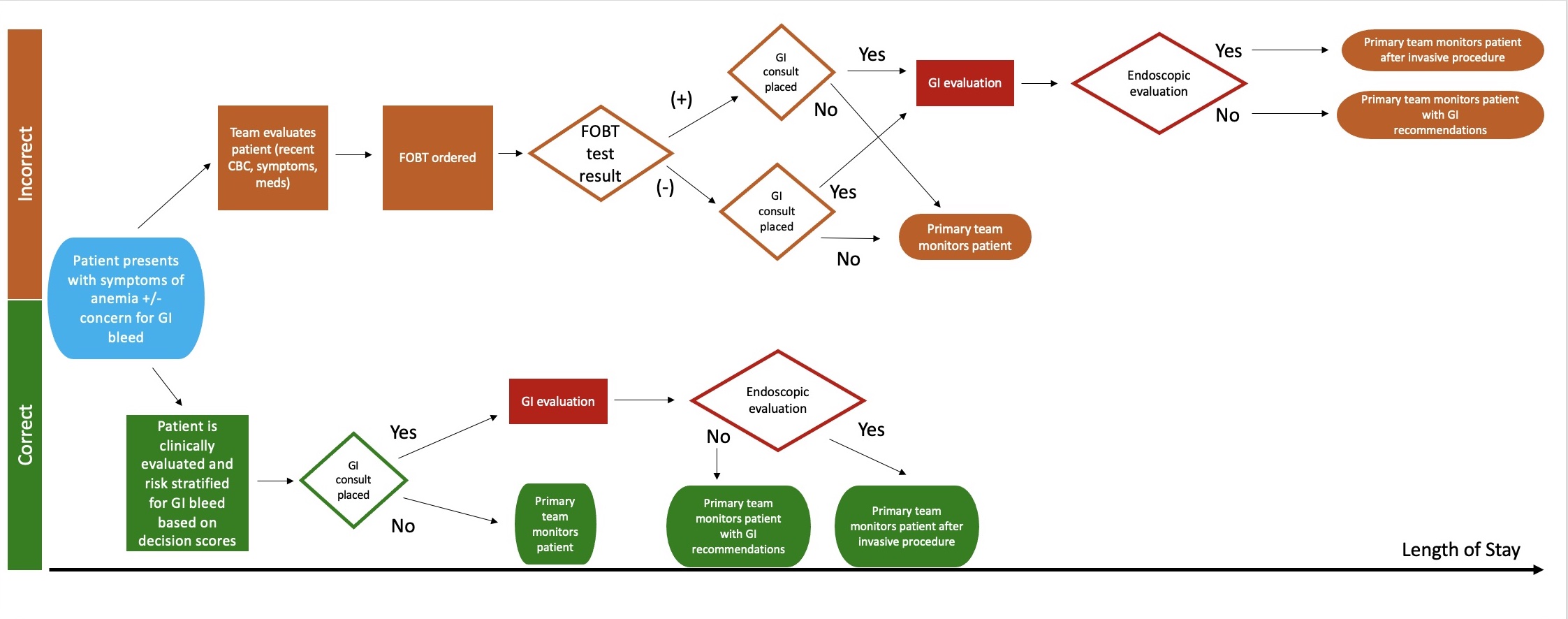
Discussion: Most FOBT were ordered by medicine providers and almost a third were ordered despite overt GI bleed. Although patients with a positive FOBT were more likely to receive a GI consult, 28% with negative FOBT still had a GI consult, suggesting FOBT was not reliable in deciding the next step and as seen in our process map in Figure 1, may have delayed care. In those that underwent endoscopy, we found no difference in the number of patients with acute cause of bleeding between those in the positive and negative groups (p = 0. 127). GI was not consulted in 11 patients that had overt bleed and a negative FOBT, suggesting some providers may be incorrectly relying on FOBT rather than the full clinical picture. We are currently working with hospital stakeholders to create an educational intervention to review diagnostic evaluation of inpatient GI bleeding. Future plans include restricting and eventually removing the test from the inpatient lab orders.
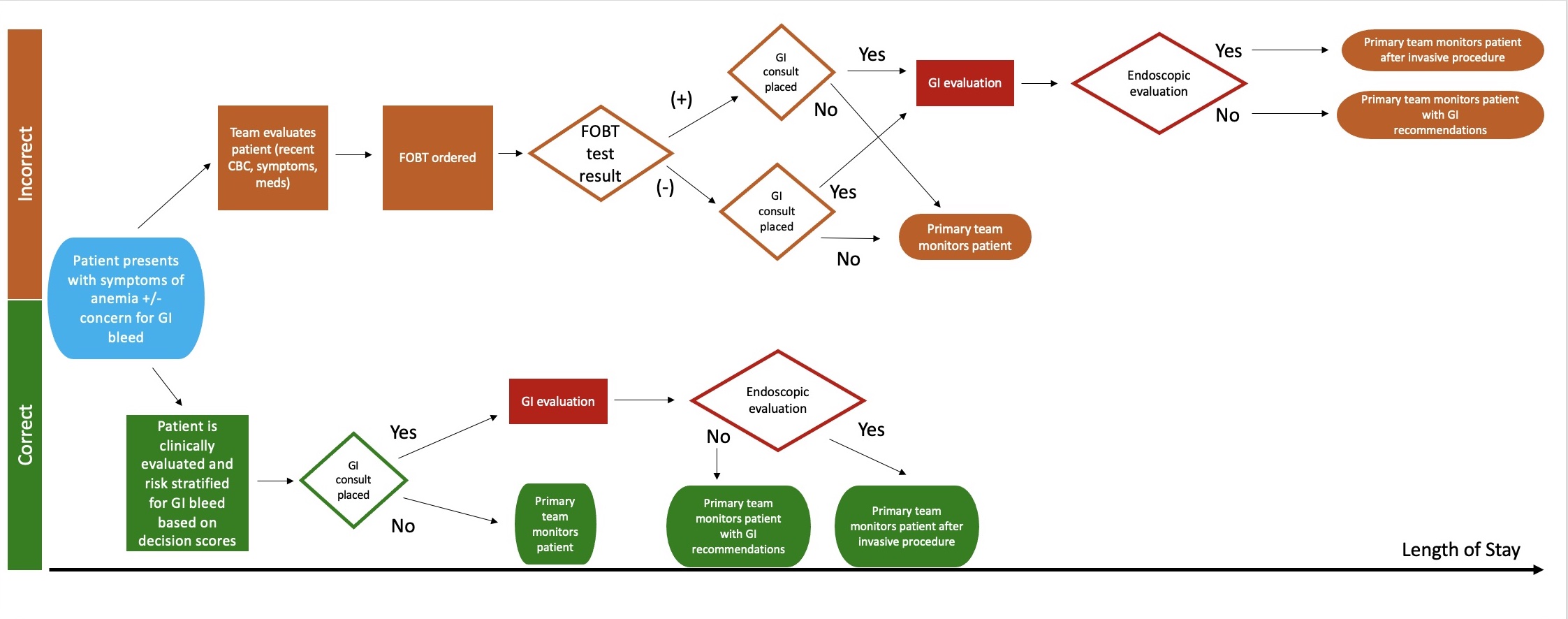
Figure: Figure 1. Process map demonstrating additional steps taken in evaluation of anemia and/or gastrointestinal bleeding with FOBT usage as compared to standard of care.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Neelima Gaddipati indicated no relevant financial relationships.
Sirisha Gaddipati indicated no relevant financial relationships.
Hua Li indicated no relevant financial relationships.
Ami Panara Shukla indicated no relevant financial relationships.
Neelima Gaddipati, MD, MBA1, Sirisha Gaddipati, MD2, Hua Li, MS, MD, PhD3, Ami Panara Shukla, MD2. P0752 - Reducing Use of Inpatient FOBT at an Academic Tertiary Medical Center: A Quality Improvement Project, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

