Sunday Poster Session
Category: GI Bleeding
P0753 - Efficacy and Safety of Hormonal Therapy in the Treatment of Bleeding From Gastrointestinal Vascular Malformations: A Systematic Review and Meta-Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Nihal Ijaz I. Khan, MD
AdventHealth Medical Group, AdventHealth
Orlando, FL
Presenting Author(s)
Nihal I. Khan, MD1, Abdullah Javed, MBBS2, Syed Hamaad Rahman, DO3, Nouman Shafique, MD1, Abu Hurairah, MD1
1AdventHealth Medical Group, AdventHealth, Orlando, FL; 2Jinnah Hospital, Lahore, Punjab, Pakistan; 3Methodist Dallas Medical Center, Irving, TX
Introduction: Vascular malformations of the GI tract present a clinical challenge due to their propensity to bleed recurrently and the difficulty endoscopists face with achieving hemostasis. Hormonal therapies, including estrogens and progestins, have been used in the management of these bleeds with variable success. This systematic review examines the effectiveness of hormonal therapy in managing bleeding from GI vascular malformations.
Methods: A systematic review of the literature from MEDLINE, EMBASE and Scopus was conducted from inception to March 2024, for studies reporting on estrogen and progestin-based hormonal therapies for treating GI bleeding from vascular malformations. Outcomes of interest were the mean number of packed red blood cell (PRBC) transfusions and mean hemoglobin levels before and after hormone therapy, as well as adverse events at follow-up. Standard meta-analysis methods were followed using the random-effects model. Heterogeneity was assessed using the I2% statistics.
Results: Five studies were identified; 1 study was a multicenter randomized placebo-controlled trial, 2 were single-center single-arm clinical trials, 1 was a single-center cross-over trial and 1 was a single-center prospective cohort study. In total, 165 patients (53.9% female) were included. Bleeding sources included angiodysplasia in 3 studies, gastric antral vascular ectasia in 1 study, and vascular malformations of the GI tract in 1 study.
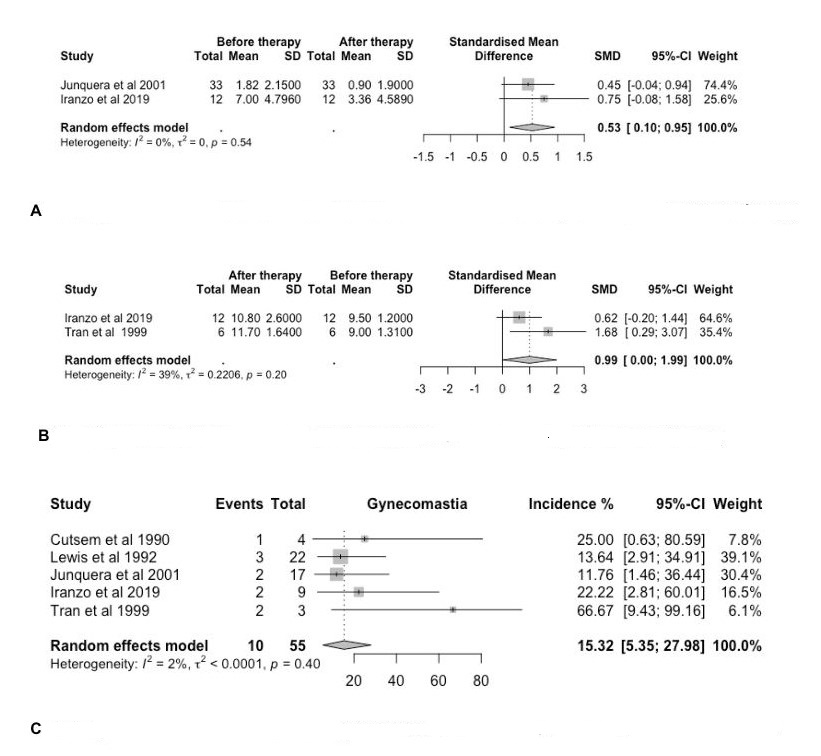
To analyze pre- and post-hormone therapy PRBC transfusions, we compared Junquera et al (2001) treatment arm with Iranzo et al (2019). The standardized mean difference (SMD) was 0.53 (95% CI 0.1 - 0.95, p=0.54, I2: 0%). Pre- and post-hormone therapy mean hemoglobin levels between Iranzo et al (2019) and Tran et al (1999) had SMD of 0.99 (95% CI 0.00 - 1.99, p=0.20, I2: 39%). The most common adverse events were gynecomastia in males (pooled rate 15.32%, 95% CI 5.35 - 27.98, I2:2%) and vaginal bleeding in females (pooled rate 20.21%, 95% CI 9.09 - 33.53, I2:0%). Results are summarized in Figure 1.
Discussion: These findings suggest that hormonal therapy may show a trend toward decreased need for PRBC transfusions and increased mean hemoglobin levels, though our results are not statistically significant. However, hormonal therapy is associated with increased risks of vaginal bleeding in females and gynecomastia in males. Further research, particularly more randomized controlled trials, are warranted to establish a clear benefit for hormonal therapy in GI bleeding.
Disclosures:
Nihal I. Khan, MD1, Abdullah Javed, MBBS2, Syed Hamaad Rahman, DO3, Nouman Shafique, MD1, Abu Hurairah, MD1. P0753 - Efficacy and Safety of Hormonal Therapy in the Treatment of Bleeding From Gastrointestinal Vascular Malformations: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1AdventHealth Medical Group, AdventHealth, Orlando, FL; 2Jinnah Hospital, Lahore, Punjab, Pakistan; 3Methodist Dallas Medical Center, Irving, TX
Introduction: Vascular malformations of the GI tract present a clinical challenge due to their propensity to bleed recurrently and the difficulty endoscopists face with achieving hemostasis. Hormonal therapies, including estrogens and progestins, have been used in the management of these bleeds with variable success. This systematic review examines the effectiveness of hormonal therapy in managing bleeding from GI vascular malformations.
Methods: A systematic review of the literature from MEDLINE, EMBASE and Scopus was conducted from inception to March 2024, for studies reporting on estrogen and progestin-based hormonal therapies for treating GI bleeding from vascular malformations. Outcomes of interest were the mean number of packed red blood cell (PRBC) transfusions and mean hemoglobin levels before and after hormone therapy, as well as adverse events at follow-up. Standard meta-analysis methods were followed using the random-effects model. Heterogeneity was assessed using the I2% statistics.
Results: Five studies were identified; 1 study was a multicenter randomized placebo-controlled trial, 2 were single-center single-arm clinical trials, 1 was a single-center cross-over trial and 1 was a single-center prospective cohort study. In total, 165 patients (53.9% female) were included. Bleeding sources included angiodysplasia in 3 studies, gastric antral vascular ectasia in 1 study, and vascular malformations of the GI tract in 1 study.
To analyze pre- and post-hormone therapy PRBC transfusions, we compared Junquera et al (2001) treatment arm with Iranzo et al (2019). The standardized mean difference (SMD) was 0.53 (95% CI 0.1 - 0.95, p=0.54, I2: 0%). Pre- and post-hormone therapy mean hemoglobin levels between Iranzo et al (2019) and Tran et al (1999) had SMD of 0.99 (95% CI 0.00 - 1.99, p=0.20, I2: 39%). The most common adverse events were gynecomastia in males (pooled rate 15.32%, 95% CI 5.35 - 27.98, I2:2%) and vaginal bleeding in females (pooled rate 20.21%, 95% CI 9.09 - 33.53, I2:0%). Results are summarized in Figure 1.
Discussion: These findings suggest that hormonal therapy may show a trend toward decreased need for PRBC transfusions and increased mean hemoglobin levels, though our results are not statistically significant. However, hormonal therapy is associated with increased risks of vaginal bleeding in females and gynecomastia in males. Further research, particularly more randomized controlled trials, are warranted to establish a clear benefit for hormonal therapy in GI bleeding.
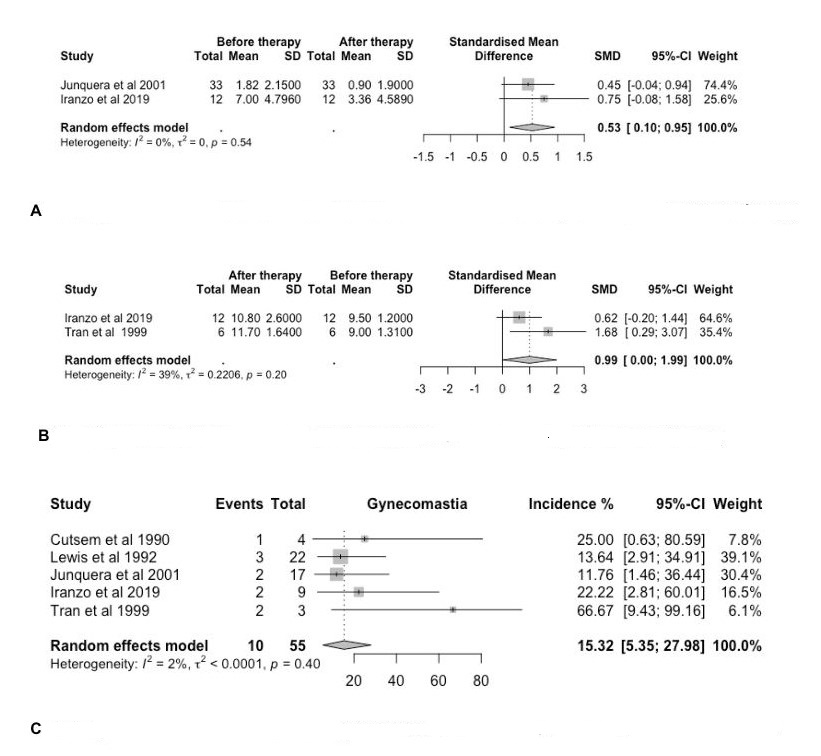
Figure: Figure 1. A. Forest plot of the SMD between mean number of PRBC transfusions pre- and post-hormone therapy. B. Forest plot of the SMD between mean hemoglobin levels pre- and post-hormone therapy. C. Forest plot of the pooled incidence of gynecomastia in male patients receiving hormone therapy
Disclosures:
Nihal Khan indicated no relevant financial relationships.
Abdullah Javed indicated no relevant financial relationships.
Syed Hamaad Rahman indicated no relevant financial relationships.
Nouman Shafique indicated no relevant financial relationships.
Abu Hurairah indicated no relevant financial relationships.
Nihal I. Khan, MD1, Abdullah Javed, MBBS2, Syed Hamaad Rahman, DO3, Nouman Shafique, MD1, Abu Hurairah, MD1. P0753 - Efficacy and Safety of Hormonal Therapy in the Treatment of Bleeding From Gastrointestinal Vascular Malformations: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
