Sunday Poster Session
Category: GI Bleeding
P0754 - Gastrointestinal Amyloidosis: A Case Report
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- OA
Oluwatayo J. Awolumate, MD
Howard University Hospital
Washington, MD
Presenting Author(s)
Oluwatayo J. Awolumate, MD, Kristen Miller, MD, Lakshmi Chirumamilla, MD, Adeyinka O. Laiyemo, MD, MPH, Angesom Kibreab, MD, Farshad Aduli, MD
Howard University Hospital, Washington, DC
Introduction: Amyloidosis is a heterogeneous group of diseases in which the extracellular deposition of abnormal fibrillar proteins disrupts tissue structure and function [1]. Each type of amyloidosis shows varying predilections to deposit in target organs, with AA amyloidosis showing the highest rates of gastrointestinal (GI) manifestations at 10%–70% [2]. GI involvement in AL amyloidosis is defined as the presence of gastrointestinal symptoms with direct biopsy verification [3]. The symptoms include diarrhea, steatorrhea, or constipation; pseudo-obstruction; and hepatic involvement ranging from mild hepatomegaly to an elevated alkaline phosphatase level [3,4]. In up to 57% of cases of systemic amyloidosis, ulcerations, erosions, or amyloidoma ulcers can cause gastrointestinal bleeding [5].
Case Description/Methods: We present a case of a 66-year-old male who presented with acute onset, generalized body weakness, shortness of breath, dizziness, and episodes of black tarry stool prior to presentation. He was recently hospitalized for symptomatic anemia without any active bleeding source. His hemoglobin was 4.4 g/dl, necessitating blood transfusion.
The examination findings at the time of presentation revealed an anemic patient who was in respiratory distress, afebrile, and had a hemoglobin level of 4.6 g/dl. The patient was resuscitated with IV fluid hydration, given high-dose intravenous proton pump inhibitor, and transfused with four units of packed red blood cells, which improved his hemoglobin level to 9.4 g/dl. He had an upper and lower endoscopy, with findings revealing localized non-bleeding friable erosions with superficial ulcerations in the lesser curvature of the stomach. A biopsy revealed amyloid deposits in the submucosal tissue and vessel wall, chronic inflammation and focal erosion in the gastric body and antrum, as well as intestinal metaplasia in the antrum. Duodenal biopsy also revealed mucosa with focal amyloid deposits. Congo red staining showed polarizable amyloid deposition. The patient's clinical condition improved, and he was discharged after four days on admission as he was deemed medically stable for discharge.
Discussion: Our case report further emphasizes the importance of considering amyloidosis in the differential diagnosis of GI symptoms, especially when they are persistent and accompanied by other systemic signs. A high index of suspicion, endoscopic, and histological confirmation through biopsies are essential in making a diagnosis.
Disclosures:
Oluwatayo J. Awolumate, MD, Kristen Miller, MD, Lakshmi Chirumamilla, MD, Adeyinka O. Laiyemo, MD, MPH, Angesom Kibreab, MD, Farshad Aduli, MD. P0754 - Gastrointestinal Amyloidosis: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Howard University Hospital, Washington, DC
Introduction: Amyloidosis is a heterogeneous group of diseases in which the extracellular deposition of abnormal fibrillar proteins disrupts tissue structure and function [1]. Each type of amyloidosis shows varying predilections to deposit in target organs, with AA amyloidosis showing the highest rates of gastrointestinal (GI) manifestations at 10%–70% [2]. GI involvement in AL amyloidosis is defined as the presence of gastrointestinal symptoms with direct biopsy verification [3]. The symptoms include diarrhea, steatorrhea, or constipation; pseudo-obstruction; and hepatic involvement ranging from mild hepatomegaly to an elevated alkaline phosphatase level [3,4]. In up to 57% of cases of systemic amyloidosis, ulcerations, erosions, or amyloidoma ulcers can cause gastrointestinal bleeding [5].
Case Description/Methods: We present a case of a 66-year-old male who presented with acute onset, generalized body weakness, shortness of breath, dizziness, and episodes of black tarry stool prior to presentation. He was recently hospitalized for symptomatic anemia without any active bleeding source. His hemoglobin was 4.4 g/dl, necessitating blood transfusion.
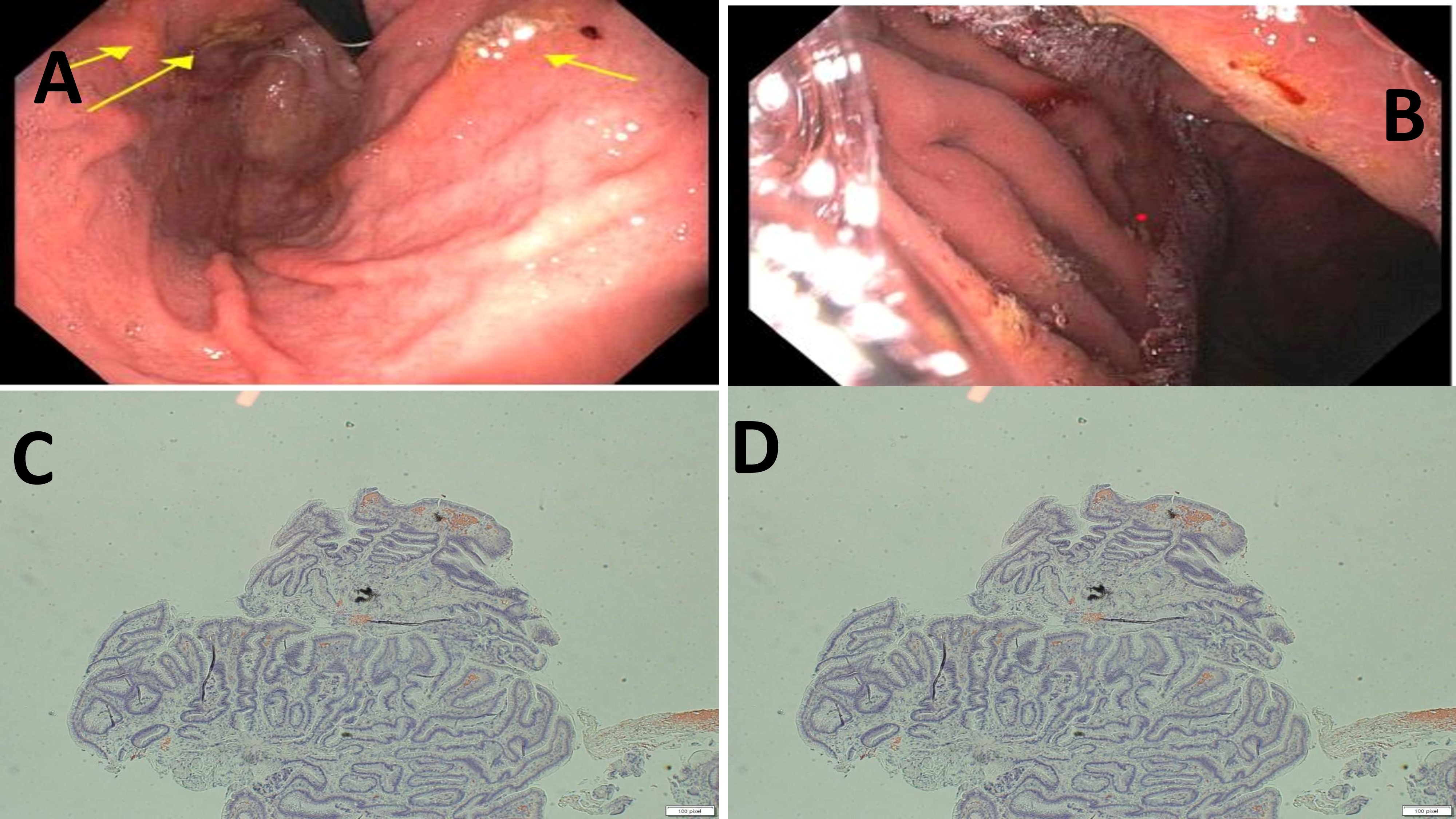
The examination findings at the time of presentation revealed an anemic patient who was in respiratory distress, afebrile, and had a hemoglobin level of 4.6 g/dl. The patient was resuscitated with IV fluid hydration, given high-dose intravenous proton pump inhibitor, and transfused with four units of packed red blood cells, which improved his hemoglobin level to 9.4 g/dl. He had an upper and lower endoscopy, with findings revealing localized non-bleeding friable erosions with superficial ulcerations in the lesser curvature of the stomach. A biopsy revealed amyloid deposits in the submucosal tissue and vessel wall, chronic inflammation and focal erosion in the gastric body and antrum, as well as intestinal metaplasia in the antrum. Duodenal biopsy also revealed mucosa with focal amyloid deposits. Congo red staining showed polarizable amyloid deposition. The patient's clinical condition improved, and he was discharged after four days on admission as he was deemed medically stable for discharge.
Discussion: Our case report further emphasizes the importance of considering amyloidosis in the differential diagnosis of GI symptoms, especially when they are persistent and accompanied by other systemic signs. A high index of suspicion, endoscopic, and histological confirmation through biopsies are essential in making a diagnosis.
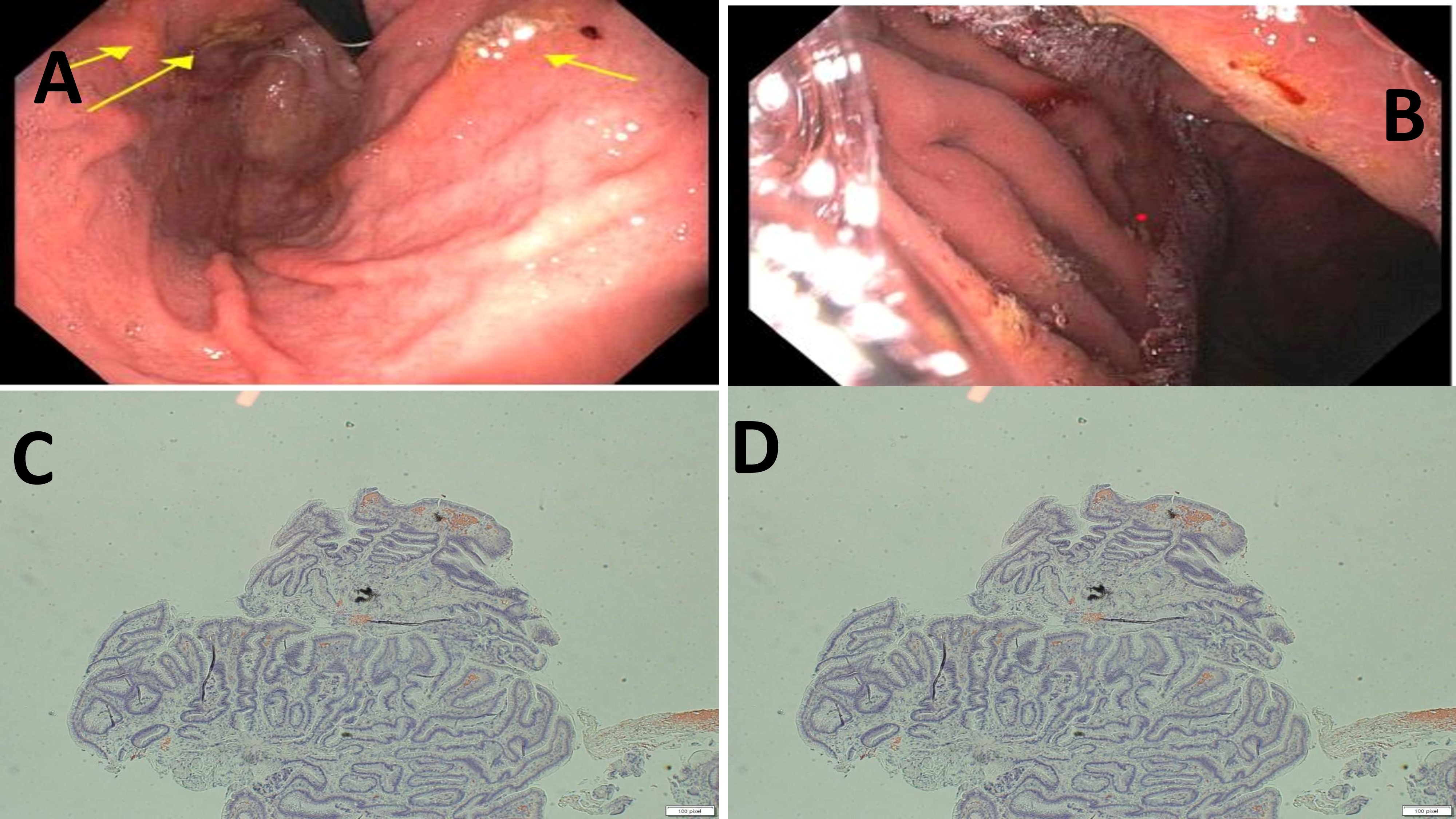
Figure: Figures A and B showing gastric fundus with erosive gastropathy, Figures C and D showing gastric biopsy report with Congo-red staining showing polarizable amyloid deposition.
Disclosures:
Oluwatayo Awolumate indicated no relevant financial relationships.
Kristen Miller indicated no relevant financial relationships.
Lakshmi Chirumamilla indicated no relevant financial relationships.
Adeyinka Laiyemo indicated no relevant financial relationships.
Angesom Kibreab indicated no relevant financial relationships.
Farshad Aduli indicated no relevant financial relationships.
Oluwatayo J. Awolumate, MD, Kristen Miller, MD, Lakshmi Chirumamilla, MD, Adeyinka O. Laiyemo, MD, MPH, Angesom Kibreab, MD, Farshad Aduli, MD. P0754 - Gastrointestinal Amyloidosis: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
