Sunday Poster Session
Category: GI Bleeding
P0758 - Gastrointestinal Bleeding in a Kidney Transplant Recipient
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Michael Vutam, DO
Willis-Knighton Health System
Shreveport, LA
Presenting Author(s)
Michael Vutam, DO1, Navneet Kaur, MD1, Guillermo Padilla, MD1, Neeraj Singh, MD2
1Willis-Knighton Health System, Shreveport, LA; 2Willis Knighton Health System, Shreveport, LA
Introduction: Opportunistic infections are common in transplant recipients, but gastrointestinal bleed is rarely reported to be due to opportunistic fungal infections, and hence could present as a diagnostic challenge. We report a case of disseminated histoplasmosis in a kidney transplant recipient whose initial presentation was acute lower gastrointestinal bleeding with no other symptoms. The colonoscopy showed scattered punched-out circular colonic ulcers with biopsy revealing budding yeasts consistent with a diagnosis of histoplasmosis.
This case highlights the importance of considering histoplasmosis in the differential diagnosis of GI bleed and diarrhea in the solid organ transplant recipients.
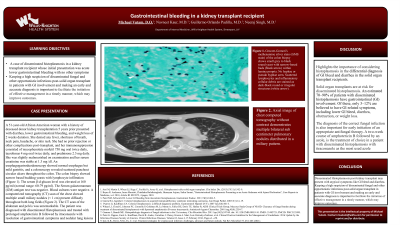
Case Description/Methods: A 51-year-old woman with a history of deceased donor kidney transplantation 5 years prior presented with diarrhea, lower gastrointestinal bleeding, and weight loss of 2 weeks duration. She denied any fever, shortness of breath, headache, or skin rash. She had no prior rejection or other complications post-transplant, and her immunosuppression consisted of mycophenolate mofetil 750 mg oral twice daily, tacrolimus 4 mg oral twice daily, and prednisone 2.5 mg daily. She was slightly malnourished on examination and her serum creatinine was stable at 1.3 mg/dl. An EGD showed normal esophagus but mild gastritis, and a colonoscopy revealed scattered punched-out circular ulcers throughout the colon. The colon biopsy showed narrow based budding yeasts with lymphocyte infiltration. The serum β-d-glucan level was elevated at 160 pg/ml (normal range: 60-79 pg/ml). The Serum galactomannan (GM) antigen test was negative. Blood cultures were negative. A computerized tomography (CT) scan of the chest showed multiple small miliary nodules (< 1 cm) present diffusely throughout both lung fields. The CT scan of the abdomen and pelvis was unremarkable. The patient was diagnosed with disseminated histoplasmosis and treated with prolonged Amphotericin B followed by Itraconazole with resolution of gastrointestinal symptoms and nodular lung lesions.
Discussion: Highlights the importance of considering histoplasmosis in the differential diagnosis of GI bleed and diarrhea in the solid organ transplant recipients. Solid organ transplants are at risk for disseminated histoplasmosis. An estimated 70–90% of patients with disseminated histoplasmosis have gastrointestinal (GI) involvement. Of these, only 3–12% are believed to have GI-related symptoms, including lower GI bleed, diarrhea, obstruction, or weight loss.

Disclosures:
Michael Vutam, DO1, Navneet Kaur, MD1, Guillermo Padilla, MD1, Neeraj Singh, MD2. P0758 - Gastrointestinal Bleeding in a Kidney Transplant Recipient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Willis-Knighton Health System, Shreveport, LA; 2Willis Knighton Health System, Shreveport, LA
Introduction: Opportunistic infections are common in transplant recipients, but gastrointestinal bleed is rarely reported to be due to opportunistic fungal infections, and hence could present as a diagnostic challenge. We report a case of disseminated histoplasmosis in a kidney transplant recipient whose initial presentation was acute lower gastrointestinal bleeding with no other symptoms. The colonoscopy showed scattered punched-out circular colonic ulcers with biopsy revealing budding yeasts consistent with a diagnosis of histoplasmosis.
This case highlights the importance of considering histoplasmosis in the differential diagnosis of GI bleed and diarrhea in the solid organ transplant recipients.
Case Description/Methods: A 51-year-old woman with a history of deceased donor kidney transplantation 5 years prior presented with diarrhea, lower gastrointestinal bleeding, and weight loss of 2 weeks duration. She denied any fever, shortness of breath, headache, or skin rash. She had no prior rejection or other complications post-transplant, and her immunosuppression consisted of mycophenolate mofetil 750 mg oral twice daily, tacrolimus 4 mg oral twice daily, and prednisone 2.5 mg daily. She was slightly malnourished on examination and her serum creatinine was stable at 1.3 mg/dl. An EGD showed normal esophagus but mild gastritis, and a colonoscopy revealed scattered punched-out circular ulcers throughout the colon. The colon biopsy showed narrow based budding yeasts with lymphocyte infiltration. The serum β-d-glucan level was elevated at 160 pg/ml (normal range: 60-79 pg/ml). The Serum galactomannan (GM) antigen test was negative. Blood cultures were negative. A computerized tomography (CT) scan of the chest showed multiple small miliary nodules (< 1 cm) present diffusely throughout both lung fields. The CT scan of the abdomen and pelvis was unremarkable. The patient was diagnosed with disseminated histoplasmosis and treated with prolonged Amphotericin B followed by Itraconazole with resolution of gastrointestinal symptoms and nodular lung lesions.
Discussion: Highlights the importance of considering histoplasmosis in the differential diagnosis of GI bleed and diarrhea in the solid organ transplant recipients. Solid organ transplants are at risk for disseminated histoplasmosis. An estimated 70–90% of patients with disseminated histoplasmosis have gastrointestinal (GI) involvement. Of these, only 3–12% are believed to have GI-related symptoms, including lower GI bleed, diarrhea, obstruction, or weight loss.

Figure: Axial image of chest computed tomography without contrast demonstrates multiple bilateral sub centimeter pulmonary nodules distributed in a miliary pattern.
Disclosures:
Michael Vutam indicated no relevant financial relationships.
Navneet Kaur indicated no relevant financial relationships.
Guillermo Padilla indicated no relevant financial relationships.
Neeraj Singh indicated no relevant financial relationships.
Michael Vutam, DO1, Navneet Kaur, MD1, Guillermo Padilla, MD1, Neeraj Singh, MD2. P0758 - Gastrointestinal Bleeding in a Kidney Transplant Recipient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
