Sunday Poster Session
Category: GI Bleeding
P0761 - A Case of Acute Gastrointestinal Bleeding Secondary to Acquired Hemophilia A
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Yasir Ahmed, MD
United Health Services
Binghamton, NY
Presenting Author(s)
Yasir Ahmed, MD1, Moheudin Khan, MD2, Nour Gafsi, BSc3, Usama Sakhawat, MD2, Amine Hila, MD4, Toseef Javaid, MD1
1United Health Services, Binghamton, NY; 2United Health Services, Wilson Medical Center, Binghamton, NY; 3United Health Services, Horseheads, NY; 4UHS, Binghamton, NY
Introduction: Acquired hemophilia A (AHA) is caused by the production of auto-antibodies that inhibit the coagulant activity of factor VIII. The estimated incidence of AHA in the United States is 0.2 to 1.0 case per million per year, but this incidence might be underestimated due to the difficulty in making the diagnosis.
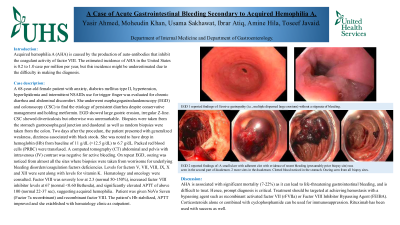
Case Description/Methods: A 68-year-old female patient with anxiety, diabetes mellitus type II, hypertension, hyperlipidemia and intermittent NSAIDs use for trigger finger was evaluated for chronic diarrhea and abdominal discomfort. She underwent esophagogastroduodenoscopy (EGD) and colonoscopy (CSC) to find the etiology of persistent diarrhea despite conservative management and holding metformin. EGD showed large gastric erosion, irregular Z-line. CSC showed diverticulosis but otherwise was unremarkable. Biopsies were taken from the stomach gastroesophageal junction and duodenal as well as random biopsies were taken from the colon. Two days after the procedure, the patient presented with generalized weakness, dizziness associated with black stools. She was noted to have drop in hemoglobin (Hb) from baseline of 11 g/dL ( >12.5 g/dL) to 6.7 g/dL. Packed red blood cells (PRBC) were transfused. A computed tomography (CT) abdominal and pelvis with intravenous (IV) contrast was negative for active bleeding. On repeat EGD, oozing was noticed from almost all the sites where biopsies were taken from worrisome for underlying bleeding disorders/coagulation factors deficiencies. Levels for factors V, VII, VIII, IX, X and XII were sent along with levels for vitamin K. Hematology and oncology were consulted. Factor VIII was severely low at 2.3 (normal 50-150%), increased factor VIII inhibitor levels at 67 (normal < 0.60 Bethesda), and significantly elevated APTT of above 100 (normal 22-37 sec), suggesting acquired hemophilia. Patient was given NoVo Seven (Factor 7a recombinant) and recombinant factor VIII. The patient’s Hb stabilized, APTT improved and she established with hematology clinic as outpatient.
Discussion: AHA is associated with significant mortality (7-22%) as it can lead to life-threatening gastrointestinal bleeding, and is difficult to treat. Hence, prompt diagnosis is critical. Treatment should be targeted at achieving hemostasis with a bypassing agent such as recombinant activated factor VII (rFVIIa) or Factor VIII Inhibitor Bypassing Agent (FEIBA). corticosteroids alone or combined with cyclophosphamide can be used for immunosuppression. Rituximab has been used with success as well.
Disclosures:
Yasir Ahmed, MD1, Moheudin Khan, MD2, Nour Gafsi, BSc3, Usama Sakhawat, MD2, Amine Hila, MD4, Toseef Javaid, MD1. P0761 - A Case of Acute Gastrointestinal Bleeding Secondary to Acquired Hemophilia A, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1United Health Services, Binghamton, NY; 2United Health Services, Wilson Medical Center, Binghamton, NY; 3United Health Services, Horseheads, NY; 4UHS, Binghamton, NY
Introduction: Acquired hemophilia A (AHA) is caused by the production of auto-antibodies that inhibit the coagulant activity of factor VIII. The estimated incidence of AHA in the United States is 0.2 to 1.0 case per million per year, but this incidence might be underestimated due to the difficulty in making the diagnosis.
Case Description/Methods: A 68-year-old female patient with anxiety, diabetes mellitus type II, hypertension, hyperlipidemia and intermittent NSAIDs use for trigger finger was evaluated for chronic diarrhea and abdominal discomfort. She underwent esophagogastroduodenoscopy (EGD) and colonoscopy (CSC) to find the etiology of persistent diarrhea despite conservative management and holding metformin. EGD showed large gastric erosion, irregular Z-line. CSC showed diverticulosis but otherwise was unremarkable. Biopsies were taken from the stomach gastroesophageal junction and duodenal as well as random biopsies were taken from the colon. Two days after the procedure, the patient presented with generalized weakness, dizziness associated with black stools. She was noted to have drop in hemoglobin (Hb) from baseline of 11 g/dL ( >12.5 g/dL) to 6.7 g/dL. Packed red blood cells (PRBC) were transfused. A computed tomography (CT) abdominal and pelvis with intravenous (IV) contrast was negative for active bleeding. On repeat EGD, oozing was noticed from almost all the sites where biopsies were taken from worrisome for underlying bleeding disorders/coagulation factors deficiencies. Levels for factors V, VII, VIII, IX, X and XII were sent along with levels for vitamin K. Hematology and oncology were consulted. Factor VIII was severely low at 2.3 (normal 50-150%), increased factor VIII inhibitor levels at 67 (normal < 0.60 Bethesda), and significantly elevated APTT of above 100 (normal 22-37 sec), suggesting acquired hemophilia. Patient was given NoVo Seven (Factor 7a recombinant) and recombinant factor VIII. The patient’s Hb stabilized, APTT improved and she established with hematology clinic as outpatient.
Discussion: AHA is associated with significant mortality (7-22%) as it can lead to life-threatening gastrointestinal bleeding, and is difficult to treat. Hence, prompt diagnosis is critical. Treatment should be targeted at achieving hemostasis with a bypassing agent such as recombinant activated factor VII (rFVIIa) or Factor VIII Inhibitor Bypassing Agent (FEIBA). corticosteroids alone or combined with cyclophosphamide can be used for immunosuppression. Rituximab has been used with success as well.
Disclosures:
Yasir Ahmed indicated no relevant financial relationships.
Moheudin Khan indicated no relevant financial relationships.
Nour Gafsi indicated no relevant financial relationships.
Usama Sakhawat indicated no relevant financial relationships.
Amine Hila indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Yasir Ahmed, MD1, Moheudin Khan, MD2, Nour Gafsi, BSc3, Usama Sakhawat, MD2, Amine Hila, MD4, Toseef Javaid, MD1. P0761 - A Case of Acute Gastrointestinal Bleeding Secondary to Acquired Hemophilia A, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
