Sunday Poster Session
Category: GI Bleeding
P0764 - Cocaine-Related Colitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- MA
Mohamed Ahmed, MD
CarePoint Health - Bayonne Medical Center
Jersey City, NJ
Presenting Author(s)
Mohamed Ahmed, MD1, Adwait Patel, MD2, John Hahn, MD2
1CarePoint Health - Bayonne Medical Center, Jersey City, NJ; 2CarePoint Health - Bayonne Medical Center, Bayonne, NJ
Introduction: Cocaine use is rising in persons ≥50 years old and in socioeconomically disadvantaged communities. Cocaine-induced bowel ischemia is uncommon but deadly with findings that have been previously described in the literature. In this report, we present a rare case of ischemic colitis secondary to active cocaine abuse in an adult female with known medical history of human immunodeficiency virus (HIV) and illicit drug use.
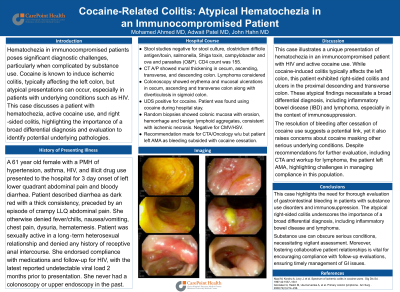
Case Description/Methods: A 61 year old female with a past medical history of HTN, asthma, HIV, illicit drug use presented to the hospital for 3 day of left lower quadrant abdominal pain and bloody diarrhea. Stool was dark red with a thick consistency and preceded by an episode of crampy abdominal pain. Patient was sexually active in a long‐term heterosexual relationship and denied any history of receptive anal intercourse. She was compliant with HAART and VL 2 months ago was undetectable. No prior EGD/Colonoscopy. Blood work showed positive HIV status, negative cryptococcus antigen, CMV PCR. Stool studies negative for infectious etiology. UDS positive for cocaine. CT Abdomen showed severe thickening in terminal ileum and cecum. Colonoscopy showed erythematous mucosa with ulcerations in cecum, ascending, transverse, and descending colon along with diverticulosis in sigmoid colon. Random biopsies showed colonic mucosa with erosion, hemorrhage and benign lymphoid aggregates, consistent with ischemic necrosis.
Discussion: Given its high mortality, cocaine-related ischemia should be considered in patients presenting with acute abdominal pain and/or rectal bleeding with evidence of bowel wall thickening or pneumatosis on imaging or colonoscopy. Our patient had prominent right colon thickening for which our initial differentials included IBD vs. right sided ischemia from an embolic source. She lacked risk factors for embolic disease as in the case of atrial fibrillation or inherited clotting disorders. The acute presentation and lack of stool frequency or diarrhea did not fully support IBD however this was to be ruled out. Routine testing for cocaine may help identify high risk patients when ischemic colitis is a part of the differential diagnoses. After cessation of cocaine, the patient's hematochezia resolved and abdominal pain improved. In conclusion, Cocaine-induced gastrointestinal injury is a life-threatening disease that requires rapid diagnosis and treatment to preclude invasive surgical management, extensive length of stay, and preventable long-term complications.

Disclosures:
Mohamed Ahmed, MD1, Adwait Patel, MD2, John Hahn, MD2. P0764 - Cocaine-Related Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1CarePoint Health - Bayonne Medical Center, Jersey City, NJ; 2CarePoint Health - Bayonne Medical Center, Bayonne, NJ
Introduction: Cocaine use is rising in persons ≥50 years old and in socioeconomically disadvantaged communities. Cocaine-induced bowel ischemia is uncommon but deadly with findings that have been previously described in the literature. In this report, we present a rare case of ischemic colitis secondary to active cocaine abuse in an adult female with known medical history of human immunodeficiency virus (HIV) and illicit drug use.
Case Description/Methods: A 61 year old female with a past medical history of HTN, asthma, HIV, illicit drug use presented to the hospital for 3 day of left lower quadrant abdominal pain and bloody diarrhea. Stool was dark red with a thick consistency and preceded by an episode of crampy abdominal pain. Patient was sexually active in a long‐term heterosexual relationship and denied any history of receptive anal intercourse. She was compliant with HAART and VL 2 months ago was undetectable. No prior EGD/Colonoscopy. Blood work showed positive HIV status, negative cryptococcus antigen, CMV PCR. Stool studies negative for infectious etiology. UDS positive for cocaine. CT Abdomen showed severe thickening in terminal ileum and cecum. Colonoscopy showed erythematous mucosa with ulcerations in cecum, ascending, transverse, and descending colon along with diverticulosis in sigmoid colon. Random biopsies showed colonic mucosa with erosion, hemorrhage and benign lymphoid aggregates, consistent with ischemic necrosis.
Discussion: Given its high mortality, cocaine-related ischemia should be considered in patients presenting with acute abdominal pain and/or rectal bleeding with evidence of bowel wall thickening or pneumatosis on imaging or colonoscopy. Our patient had prominent right colon thickening for which our initial differentials included IBD vs. right sided ischemia from an embolic source. She lacked risk factors for embolic disease as in the case of atrial fibrillation or inherited clotting disorders. The acute presentation and lack of stool frequency or diarrhea did not fully support IBD however this was to be ruled out. Routine testing for cocaine may help identify high risk patients when ischemic colitis is a part of the differential diagnoses. After cessation of cocaine, the patient's hematochezia resolved and abdominal pain improved. In conclusion, Cocaine-induced gastrointestinal injury is a life-threatening disease that requires rapid diagnosis and treatment to preclude invasive surgical management, extensive length of stay, and preventable long-term complications.

Figure: CT findings, Endoscopic findings
Disclosures:
Mohamed Ahmed indicated no relevant financial relationships.
Adwait Patel indicated no relevant financial relationships.
John Hahn indicated no relevant financial relationships.
Mohamed Ahmed, MD1, Adwait Patel, MD2, John Hahn, MD2. P0764 - Cocaine-Related Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
