Sunday Poster Session
Category: GI Bleeding
P0767 - Gastric Ulcer Hemorrhage from a Gastro-Gastric LAMS Stent Placed for an EDGE Procedure
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Alec I. Sahagian, BS
Touro University Nevada
Presenting Author(s)
Alec I. Sahagian, BS1, Chris Pace, DO2, Scott Diamond, DO2, Vishvinder Sharma, MD2
1Touro University Nevada, Irvine, CA; 2Valley Hospital Medical Center, Las Vegas, NV
Introduction: Roux-en-Y gastric bypass (RYGB) complicates endoscopic access to the pancreaticobiliary tree. Endoscopic ultrasound-directed trans-gastric ERCP (EDGE) permits access to the biliary tree in RYGB patients by creating a fistulous tract between the excluded stomach and either the gastric pouch or jejunum with a lumen-apposing metal stent (LAMS). We present a case of bleeding complications following a gastro-gastric EDGE procedure.
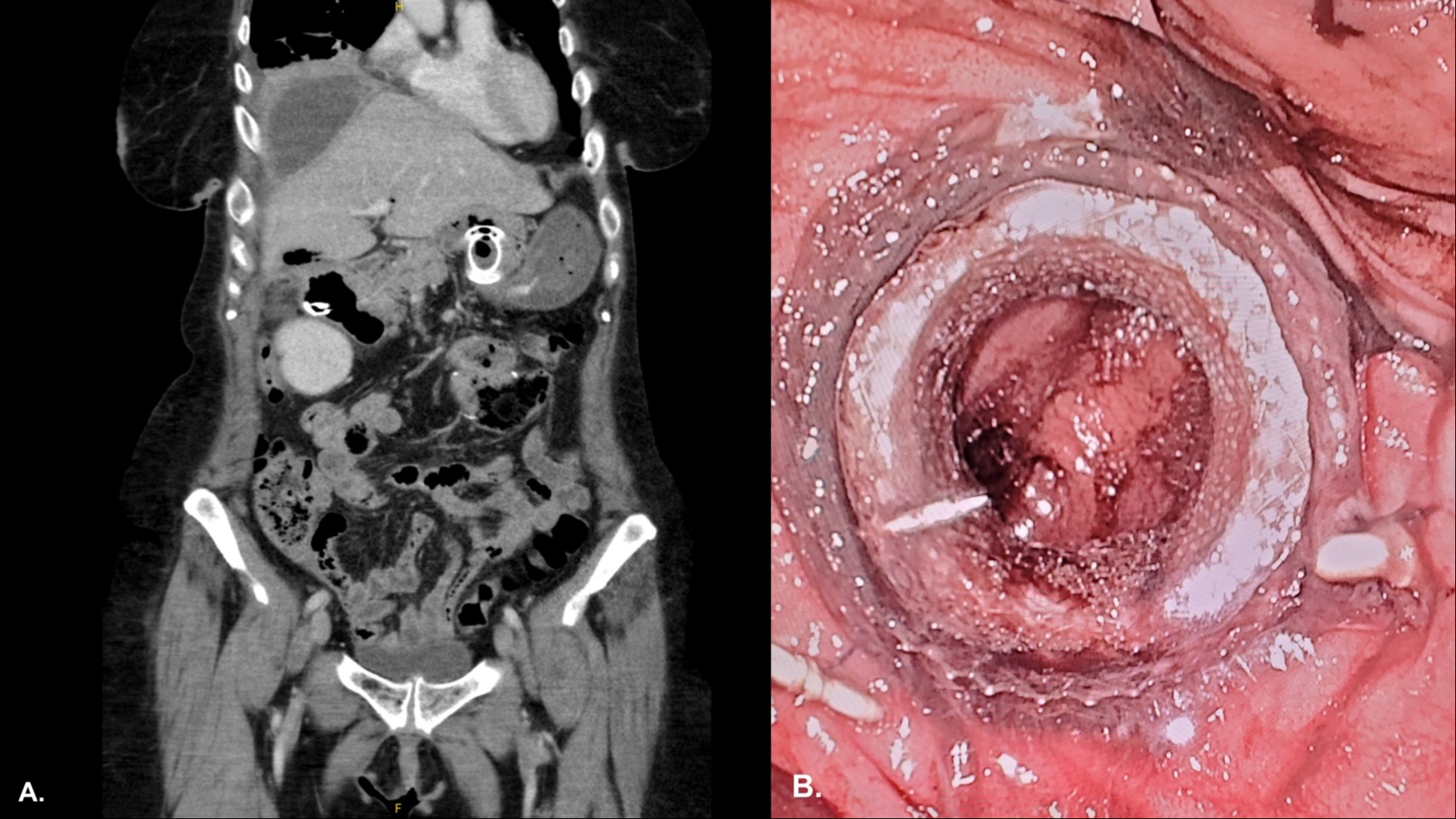
Case Description/Methods: A 62-year-old female with RYGB presents to the emergency department (ED) with hematemesis and abdominal pain. She had a cholecystectomy one month prior complicated by a high-grade bile leak requiring an IR-placed biliary drain and an EDGE procedure with biliary and pancreatic duct stent placement. She had witnessed hematemesis and melena in the ED. Initial labs show leukocytosis (15,430 WBC/mcL) and normocytic anemia (Hb 9.9g/dL). Initial vitals show tachycardia (115 BPM) and systolic hypertension (151mmHg). CT abdomen/pelvis with IV contrast showed post-surgical changes consistent with gastric bypass with marsupialization of the gastric conduit with a LAMS, a plastic CBD stent, a 15cm subdiaphragmatic fluid collection in the gallbladder fossa, and no extravasation of contrast.
Pantoprazole 40mg BID and two units of PRBCs were given. An EGD showed old blood throughout the gastric pouch and remnant stomach and several clean-based ulcers surrounding and beneath the gastro-gastric anastomosis and LAMS stent.
She had no further bleeding and was discharged on open-capsule pantoprazole.
Discussion: The clinical utility of LAMS stents is not without risk. The Food and Drug Administration (FDA) reports a 9% adverse event rate with LAMS stent use, hemorrhage being the most common (32.4%).1 Management of EDGE-related hemorrhage has been successfully managed with proton pump inhibitors (PPI), argon plasma coagulation, balloon tamponade, or stent removal.2 In some cases, prompt removal of the LAMS stent would prevent this complication; however, due to the need for a repeat ERCP with CBD stent exchange or removal, the LAMS was left in situ after the initial ERCP. Due to the known risk of hemorrhage, select patients who require prolonged gastro-gastric LAMS stents should be considered for empiric PPI for ulcer prophylaxis.
References
1. Ramai et al. Endosc Ultrasound, May 2022, 231–36
2. Ichkhanian et al. VideoGIE, June 2020, 260-63
Disclosures:
Alec I. Sahagian, BS1, Chris Pace, DO2, Scott Diamond, DO2, Vishvinder Sharma, MD2. P0767 - Gastric Ulcer Hemorrhage from a Gastro-Gastric LAMS Stent Placed for an EDGE Procedure, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Touro University Nevada, Irvine, CA; 2Valley Hospital Medical Center, Las Vegas, NV
Introduction: Roux-en-Y gastric bypass (RYGB) complicates endoscopic access to the pancreaticobiliary tree. Endoscopic ultrasound-directed trans-gastric ERCP (EDGE) permits access to the biliary tree in RYGB patients by creating a fistulous tract between the excluded stomach and either the gastric pouch or jejunum with a lumen-apposing metal stent (LAMS). We present a case of bleeding complications following a gastro-gastric EDGE procedure.
Case Description/Methods: A 62-year-old female with RYGB presents to the emergency department (ED) with hematemesis and abdominal pain. She had a cholecystectomy one month prior complicated by a high-grade bile leak requiring an IR-placed biliary drain and an EDGE procedure with biliary and pancreatic duct stent placement. She had witnessed hematemesis and melena in the ED. Initial labs show leukocytosis (15,430 WBC/mcL) and normocytic anemia (Hb 9.9g/dL). Initial vitals show tachycardia (115 BPM) and systolic hypertension (151mmHg). CT abdomen/pelvis with IV contrast showed post-surgical changes consistent with gastric bypass with marsupialization of the gastric conduit with a LAMS, a plastic CBD stent, a 15cm subdiaphragmatic fluid collection in the gallbladder fossa, and no extravasation of contrast.
Pantoprazole 40mg BID and two units of PRBCs were given. An EGD showed old blood throughout the gastric pouch and remnant stomach and several clean-based ulcers surrounding and beneath the gastro-gastric anastomosis and LAMS stent.
She had no further bleeding and was discharged on open-capsule pantoprazole.
Discussion: The clinical utility of LAMS stents is not without risk. The Food and Drug Administration (FDA) reports a 9% adverse event rate with LAMS stent use, hemorrhage being the most common (32.4%).1 Management of EDGE-related hemorrhage has been successfully managed with proton pump inhibitors (PPI), argon plasma coagulation, balloon tamponade, or stent removal.2 In some cases, prompt removal of the LAMS stent would prevent this complication; however, due to the need for a repeat ERCP with CBD stent exchange or removal, the LAMS was left in situ after the initial ERCP. Due to the known risk of hemorrhage, select patients who require prolonged gastro-gastric LAMS stents should be considered for empiric PPI for ulcer prophylaxis.
References
1. Ramai et al. Endosc Ultrasound, May 2022, 231–36
2. Ichkhanian et al. VideoGIE, June 2020, 260-63
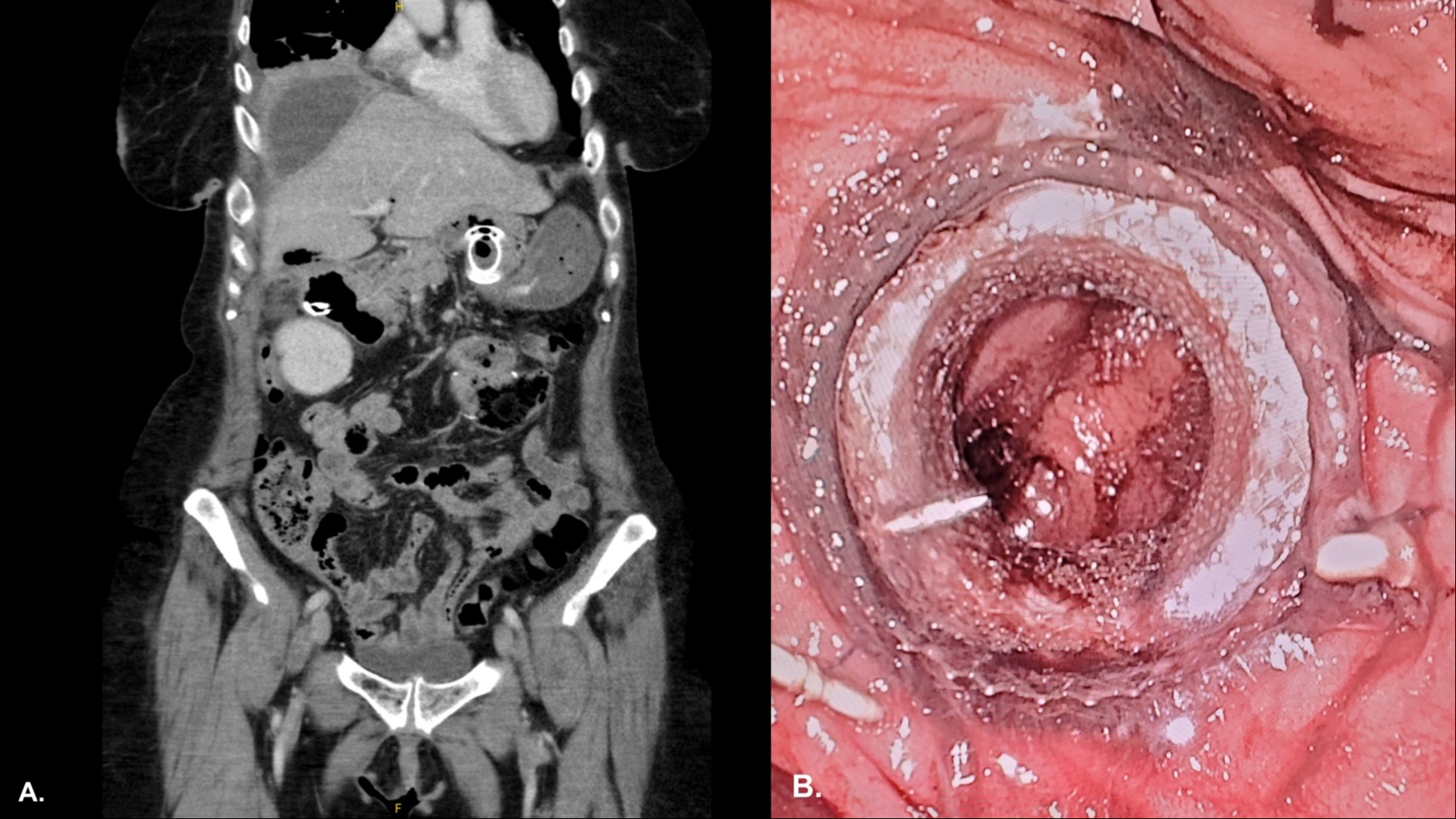
Figure: (A) CT abdomen/pelvis with IV contrast showing post-surgical changes consistent with gastric bypass with marsupialization of the gastric conduit with a LAMS, a plastic CBD stent, a 15cm subdiaphragmatic fluid collection in the gallbladder fossa, and no extravasation of contrast. (B) Endoscopic view from remnant stomach showing pale mucosa and ulcerations beneath gastro-gastric LAMS.
Disclosures:
Alec Sahagian indicated no relevant financial relationships.
Chris Pace indicated no relevant financial relationships.
Scott Diamond indicated no relevant financial relationships.
Vishvinder Sharma indicated no relevant financial relationships.
Alec I. Sahagian, BS1, Chris Pace, DO2, Scott Diamond, DO2, Vishvinder Sharma, MD2. P0767 - Gastric Ulcer Hemorrhage from a Gastro-Gastric LAMS Stent Placed for an EDGE Procedure, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
