Sunday Poster Session
Category: General Endoscopy
P0677 - Impact of Duration of GLP-1 Receptor Agonist Therapy in Endoscopic Outcomes
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Beatriz Torre, MD
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Beatriz Torre, MD1, Akash Patel, DO2, Benjamin Young, MD2, Michael J. DiMarino, MD3, Katherine Duffey, MD2, Nicholas Noverati, MD2, Charles Kistler, MD3
1Thomas Jefferson University, Philadelphia, PA; 2Thomas Jefferson University Hospital, Philadelphia, PA; 3Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
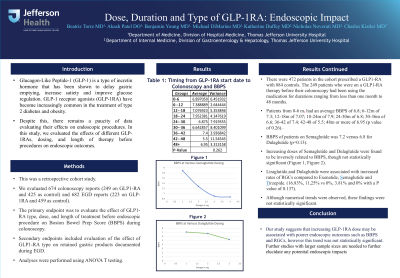
Introduction: Glucagon-Like Peptide-1 (GLP-1) is a type of incretin hormone that has been shown to delay gastric emptying, increase satiety and improve glucose regulation. GLP-1 receptor agonists (GLP-1RA) have become increasingly common for the treatment of type 2 diabetes and obesity. Despite this increase in use, there remains a paucity of data evaluating their effects on endoscopic procedures. In this study, we evaluated the effects of different GLP-1RAs, dosing, and length of therapy and its impact on endoscopic outcomes.
Methods: This was a retrospective cohort study of 674 colonoscopy reports (249 on GLP1-RA and 425 as control) and 682 EGD reports (223 on GLP-1RA and 459 as control). The primary endpoint was to evaluate the effect of GLP1-RA type, dose, and length of treatment before endoscopic procedure on Boston Bowel Prep Score (BBPS) during colonoscopy. Secondary endpoints included evaluation of the effect of GLP1-RA type on retained food documented during EGD. Analyses were performed using ANOVA T testing.
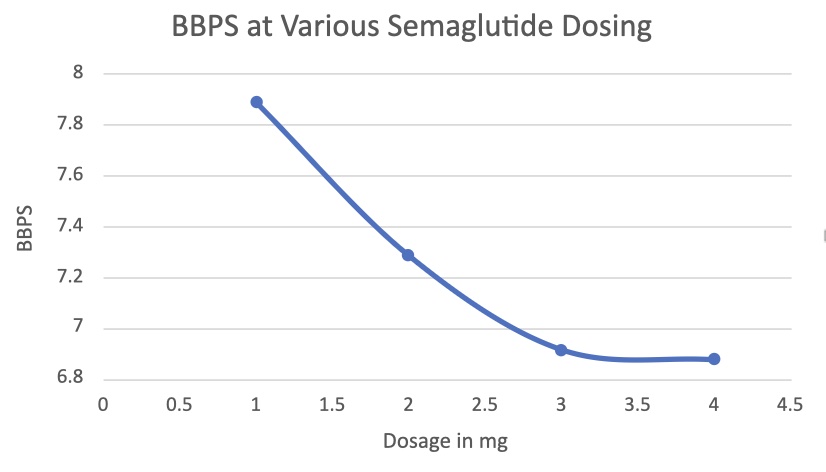
Results: There were 472 patients in the cohort prescribed a GLP1-RA with 884 controls. The 249 patients previously taking a GLP1-RA before their colonoscopy were on therapy for between from less than a month to 48 months or more (Table 2). Patients from 0-6 m had an average BBPS of 6.8; 6-12m of 7.3; 12-18m of 7.07; 18-24m of 7.9; 24-30m of 6.8; 30-36m of 6.6; 36-42 of 7.4; 42-48 of 5.5; 48m or more of 6.95 (p value of 0.26). BBPS of patients on semaglutide was 7.2 versus 6.8 for dulaglutide (p=0.13). Increased semaglutide and dulaglutide dosing were found to be inversely related to BBPS, though not statistically significant (Figure 1, Figure 2). Liraglutide and dulaglutide were associated with increased rates of EGD food retention compared to exenatide, semaglutide and tirzepatide. (16.83%, 11,25% vs 0%, 3.81% and 0% with a P value of 0.137). Although numerical trends were observed, these findings were not statistically significant.
Discussion: Our study suggests that increasing GLP-1RA dose may be associated with poorer endoscopic outcomes, but this trend was not statistically significant. The numerical trend observed, though not statistically significant, highlights the need for further research with a larger sample size/more robust methodology to explore this potential relationship.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Beatriz Torre, MD1, Akash Patel, DO2, Benjamin Young, MD2, Michael J. DiMarino, MD3, Katherine Duffey, MD2, Nicholas Noverati, MD2, Charles Kistler, MD3. P0677 - Impact of Duration of GLP-1 Receptor Agonist Therapy in Endoscopic Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Thomas Jefferson University, Philadelphia, PA; 2Thomas Jefferson University Hospital, Philadelphia, PA; 3Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction: Glucagon-Like Peptide-1 (GLP-1) is a type of incretin hormone that has been shown to delay gastric emptying, increase satiety and improve glucose regulation. GLP-1 receptor agonists (GLP-1RA) have become increasingly common for the treatment of type 2 diabetes and obesity. Despite this increase in use, there remains a paucity of data evaluating their effects on endoscopic procedures. In this study, we evaluated the effects of different GLP-1RAs, dosing, and length of therapy and its impact on endoscopic outcomes.
Methods: This was a retrospective cohort study of 674 colonoscopy reports (249 on GLP1-RA and 425 as control) and 682 EGD reports (223 on GLP-1RA and 459 as control). The primary endpoint was to evaluate the effect of GLP1-RA type, dose, and length of treatment before endoscopic procedure on Boston Bowel Prep Score (BBPS) during colonoscopy. Secondary endpoints included evaluation of the effect of GLP1-RA type on retained food documented during EGD. Analyses were performed using ANOVA T testing.
Results: There were 472 patients in the cohort prescribed a GLP1-RA with 884 controls. The 249 patients previously taking a GLP1-RA before their colonoscopy were on therapy for between from less than a month to 48 months or more (Table 2). Patients from 0-6 m had an average BBPS of 6.8; 6-12m of 7.3; 12-18m of 7.07; 18-24m of 7.9; 24-30m of 6.8; 30-36m of 6.6; 36-42 of 7.4; 42-48 of 5.5; 48m or more of 6.95 (p value of 0.26). BBPS of patients on semaglutide was 7.2 versus 6.8 for dulaglutide (p=0.13). Increased semaglutide and dulaglutide dosing were found to be inversely related to BBPS, though not statistically significant (Figure 1, Figure 2). Liraglutide and dulaglutide were associated with increased rates of EGD food retention compared to exenatide, semaglutide and tirzepatide. (16.83%, 11,25% vs 0%, 3.81% and 0% with a P value of 0.137). Although numerical trends were observed, these findings were not statistically significant.
Discussion: Our study suggests that increasing GLP-1RA dose may be associated with poorer endoscopic outcomes, but this trend was not statistically significant. The numerical trend observed, though not statistically significant, highlights the need for further research with a larger sample size/more robust methodology to explore this potential relationship.
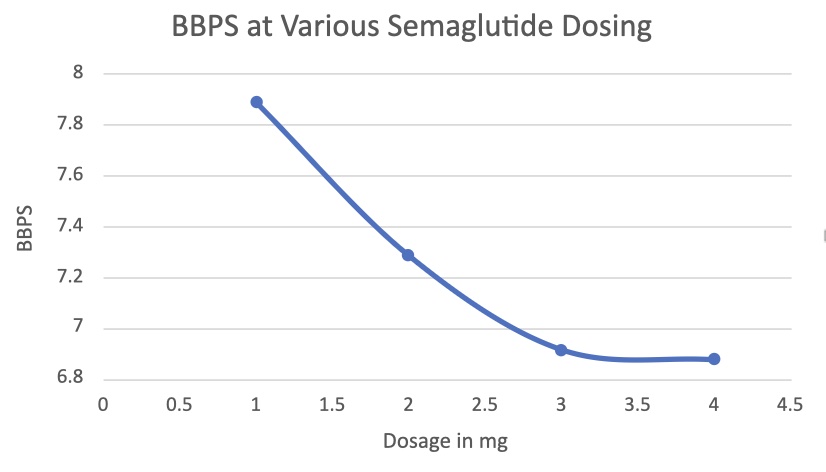
Figure: BBPS at various semaglutide doses
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Beatriz Torre indicated no relevant financial relationships.
Akash Patel indicated no relevant financial relationships.
Benjamin Young indicated no relevant financial relationships.
Michael DiMarino indicated no relevant financial relationships.
Katherine Duffey indicated no relevant financial relationships.
Nicholas Noverati indicated no relevant financial relationships.
Charles Kistler indicated no relevant financial relationships.
Beatriz Torre, MD1, Akash Patel, DO2, Benjamin Young, MD2, Michael J. DiMarino, MD3, Katherine Duffey, MD2, Nicholas Noverati, MD2, Charles Kistler, MD3. P0677 - Impact of Duration of GLP-1 Receptor Agonist Therapy in Endoscopic Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
