Sunday Poster Session
Category: Esophagus
P0612 - Statin-Induced Autoimmune Necrotizing Myositis: An Unusual Case of Dysphagia
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

John Pueringer, DO
University of Illinois College of Medicine
Chicago, IL
Presenting Author(s)
John Pueringer, DO1, Danich Qadir, MPH2, James S. Love, MD1, Hesham Elmergawy, MD1, Christopher Fernandes, MD1
1University of Illinois College of Medicine, Chicago, IL; 2Philadelphia College of Osteopathic Medicine, Philadelphia, PA
Introduction: Statin-induced autoimmune necrotizing myositis (SAINM) is characterized by muscle weakness, myalgias, elevated serum creatine kinase (CK) levels, and rarely dysphagia. We present a devastating case of SAINM, highlighting the significance of timely recognition and treatment.
Case Description/Methods: A 63-year-old male presented with dysphagia to solids and liquids for two weeks, refractory to famotidine. He also endorsed arthralgias in his shoulders, muscle aches, fatigue, dark urine, generalized weakness, and a 15 lb weight loss. He was started on Atorvastatin about one month before the symptoms began and recently finished a 7-day course of Bactrim for right lower extremity cellulitis.
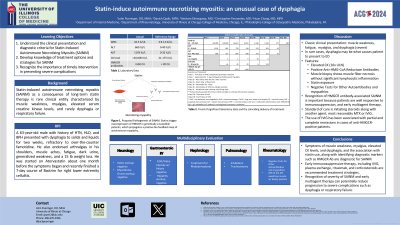
Labs were significant for a leukocytosis of 10.5 K/UL (3.9-12 K/UL), ALT of 660 U/L (0-40 U/L), AST of 1193 U/L (0-32 U/L), and CK level >20,000 U/L (21-175 U/L). The patient was started on IV fluids and admitted to the floor for non-traumatic rhabdomyolysis. Imaging and serologic work up for stroke and myasthenia gravis were negative. Endoscopy was negative for structural, infectious, and eosinophilic causes, and hepatitis workup was unremarkable. Serum aldolase, rheumatoid factor, and smooth muscle antibody were positive. MRI and biopsy of the left quadricep muscle were significant for generalized edema and necrotizing myositis with a high titer of HMG-CoA reductase antibodies to >200 U (< 20 U).
Intravenous immunoglobulin (IVIG) was initiated with dramatic reduction in his CK and transaminase levels (Table 1). Despite serologic improvement, his dysphagia and weakness worsened, and he was transferred to the ICU for respiratory failure requiring intubation. In the ICU, he received plasma exchange transfusions, rituximab, and IV steroids for treatment of necrotizing myositis. After 12 days, he had a second trial of IVIG. Following the IVIG and a prednisone taper, there was significant improvement in symptoms. He was discharged with plans to receive his next course of IVIG outpatient.
Discussion: Recognition of HMGCR antibody-associated SAINM is important because patients are well responsive to immunosuppression, and early multiagent therapy. The use of IVIG has been associated with partial and complete remissions in cases of anti-HMGCR-positive patients. Some physicians may use IVIG as a first-line therapy, particularly for patients at high risk of poor outcomes like our patient, or as monotherapy, which may be preferred in patients who are at increased risk of developing glucocorticoid-related side effects.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
John Pueringer, DO1, Danich Qadir, MPH2, James S. Love, MD1, Hesham Elmergawy, MD1, Christopher Fernandes, MD1. P0612 - Statin-Induced Autoimmune Necrotizing Myositis: An Unusual Case of Dysphagia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Illinois College of Medicine, Chicago, IL; 2Philadelphia College of Osteopathic Medicine, Philadelphia, PA
Introduction: Statin-induced autoimmune necrotizing myositis (SAINM) is characterized by muscle weakness, myalgias, elevated serum creatine kinase (CK) levels, and rarely dysphagia. We present a devastating case of SAINM, highlighting the significance of timely recognition and treatment.
Case Description/Methods: A 63-year-old male presented with dysphagia to solids and liquids for two weeks, refractory to famotidine. He also endorsed arthralgias in his shoulders, muscle aches, fatigue, dark urine, generalized weakness, and a 15 lb weight loss. He was started on Atorvastatin about one month before the symptoms began and recently finished a 7-day course of Bactrim for right lower extremity cellulitis.
Labs were significant for a leukocytosis of 10.5 K/UL (3.9-12 K/UL), ALT of 660 U/L (0-40 U/L), AST of 1193 U/L (0-32 U/L), and CK level >20,000 U/L (21-175 U/L). The patient was started on IV fluids and admitted to the floor for non-traumatic rhabdomyolysis. Imaging and serologic work up for stroke and myasthenia gravis were negative. Endoscopy was negative for structural, infectious, and eosinophilic causes, and hepatitis workup was unremarkable. Serum aldolase, rheumatoid factor, and smooth muscle antibody were positive. MRI and biopsy of the left quadricep muscle were significant for generalized edema and necrotizing myositis with a high titer of HMG-CoA reductase antibodies to >200 U (< 20 U).
Intravenous immunoglobulin (IVIG) was initiated with dramatic reduction in his CK and transaminase levels (Table 1). Despite serologic improvement, his dysphagia and weakness worsened, and he was transferred to the ICU for respiratory failure requiring intubation. In the ICU, he received plasma exchange transfusions, rituximab, and IV steroids for treatment of necrotizing myositis. After 12 days, he had a second trial of IVIG. Following the IVIG and a prednisone taper, there was significant improvement in symptoms. He was discharged with plans to receive his next course of IVIG outpatient.
Discussion: Recognition of HMGCR antibody-associated SAINM is important because patients are well responsive to immunosuppression, and early multiagent therapy. The use of IVIG has been associated with partial and complete remissions in cases of anti-HMGCR-positive patients. Some physicians may use IVIG as a first-line therapy, particularly for patients at high risk of poor outcomes like our patient, or as monotherapy, which may be preferred in patients who are at increased risk of developing glucocorticoid-related side effects.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
John Pueringer indicated no relevant financial relationships.
Danich Qadir indicated no relevant financial relationships.
James Love indicated no relevant financial relationships.
Hesham Elmergawy indicated no relevant financial relationships.
Christopher Fernandes indicated no relevant financial relationships.
John Pueringer, DO1, Danich Qadir, MPH2, James S. Love, MD1, Hesham Elmergawy, MD1, Christopher Fernandes, MD1. P0612 - Statin-Induced Autoimmune Necrotizing Myositis: An Unusual Case of Dysphagia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
