Sunday Poster Session
Category: Functional Bowel Disease
P0614 - The Burden of Pain: High Rates of Opioid and Non-Opioid Analgesic Prescription in Patients With Irritable Bowel Syndrome
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Evelyn Calderon Martinez, MD
UPMC Central PA
Harrisburg, PA
Presenting Author(s)
Evelyn Calderon Martinez, MD1, Lidia Cardelle, MS2, Adalberto Guzman, MD3, Diana Gavilanes, MD1, Shane Tripp, MS2, Julianna Kinsolving, MS2, Mauricio Alvarado, MD4, Rodrigo Villata, MD5, Anas Atras, MD1
1UPMC Central PA, Harrisburg, PA; 2Drexel University College of Medicine, Harrisburg, PA; 3University of Arkansas for Medical Sciences, Harrisburg, PA; 4University of El Salvador, San Salvador, El Salvador; 5Universidad Evangelica de El Salvador, El Salvador, San Salvador, El Salvador
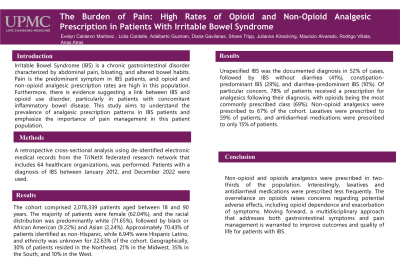
Introduction: Irritable Bowel Syndrome (IBS) is a chronic gastrointestinal disorder characterized by abdominal pain, bloating, and altered bowel habits. Pain is the predominant symptom in IBS patients, and opioid and non-opioid analgesic prescription rates are high in this population. Furthermore, there is evidence suggesting a link between IBS and opioid use disorder, particularly in patients with concomitant inflammatory bowel disease. This study aims to understand the prevalence of analgesic prescription patterns in IBS patients and emphasize the importance of pain management in this patient population.
Methods: A retrospective cross-sectional analysis using de-identified electronic medical records from the TriNetX federated research network that includes 64 healthcare organizations, was performed. Patients with a diagnosis of IBS between January 2012, and December 2022 were used.
Results: The cohort comprised 2,078,339 patients aged between 18 and 90 years. The majority of patients were female (62.04%), and the racial distribution was predominantly white (71.65%), followed by black or African American (9.22%) and Asian (2.24%). Approximately 70.43% of patients identified as non-Hispanic, while 6.94% were Hispanic Latino, and ethnicity was unknown for 22.63% of the cohort. Geographically, 30% of patients resided in the Northeast, 21% in the Midwest, 35% in the South, and 10% in the West.
Unspecified IBS was the documented diagnosis in 52% of cases, followed by IBS without diarrhea (41%), constipation-predominant IBS (29%), and diarrhea-predominant IBS (10%). Of particular concern, 78% of patients received a prescription for analgesics following their diagnosis, with opioids being the most commonly prescribed class (69%). Non-opioid analgesics were prescribed to 67% of the cohort. Laxatives were prescribed to 59% of patients, and antidiarrheal medications were prescribed to only 15% of patients.
Discussion: Non-opioid and opioids analgesics were prescribed in two-thirds of the population. Interestingly, laxatives and antidiarrheal medications were prescribed less frequently. The overreliance on opioids raises concerns regarding potential adverse effects, including opioid dependence and exacerbation of symptoms. Moving forward, a multidisciplinary approach that addresses both gastrointestinal symptoms and pain management is warranted to improve outcomes and quality of life for patients with IBS.
Disclosures:
Evelyn Calderon Martinez, MD1, Lidia Cardelle, MS2, Adalberto Guzman, MD3, Diana Gavilanes, MD1, Shane Tripp, MS2, Julianna Kinsolving, MS2, Mauricio Alvarado, MD4, Rodrigo Villata, MD5, Anas Atras, MD1. P0614 - The Burden of Pain: High Rates of Opioid and Non-Opioid Analgesic Prescription in Patients With Irritable Bowel Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1UPMC Central PA, Harrisburg, PA; 2Drexel University College of Medicine, Harrisburg, PA; 3University of Arkansas for Medical Sciences, Harrisburg, PA; 4University of El Salvador, San Salvador, El Salvador; 5Universidad Evangelica de El Salvador, El Salvador, San Salvador, El Salvador
Introduction: Irritable Bowel Syndrome (IBS) is a chronic gastrointestinal disorder characterized by abdominal pain, bloating, and altered bowel habits. Pain is the predominant symptom in IBS patients, and opioid and non-opioid analgesic prescription rates are high in this population. Furthermore, there is evidence suggesting a link between IBS and opioid use disorder, particularly in patients with concomitant inflammatory bowel disease. This study aims to understand the prevalence of analgesic prescription patterns in IBS patients and emphasize the importance of pain management in this patient population.
Methods: A retrospective cross-sectional analysis using de-identified electronic medical records from the TriNetX federated research network that includes 64 healthcare organizations, was performed. Patients with a diagnosis of IBS between January 2012, and December 2022 were used.
Results: The cohort comprised 2,078,339 patients aged between 18 and 90 years. The majority of patients were female (62.04%), and the racial distribution was predominantly white (71.65%), followed by black or African American (9.22%) and Asian (2.24%). Approximately 70.43% of patients identified as non-Hispanic, while 6.94% were Hispanic Latino, and ethnicity was unknown for 22.63% of the cohort. Geographically, 30% of patients resided in the Northeast, 21% in the Midwest, 35% in the South, and 10% in the West.
Unspecified IBS was the documented diagnosis in 52% of cases, followed by IBS without diarrhea (41%), constipation-predominant IBS (29%), and diarrhea-predominant IBS (10%). Of particular concern, 78% of patients received a prescription for analgesics following their diagnosis, with opioids being the most commonly prescribed class (69%). Non-opioid analgesics were prescribed to 67% of the cohort. Laxatives were prescribed to 59% of patients, and antidiarrheal medications were prescribed to only 15% of patients.
Discussion: Non-opioid and opioids analgesics were prescribed in two-thirds of the population. Interestingly, laxatives and antidiarrheal medications were prescribed less frequently. The overreliance on opioids raises concerns regarding potential adverse effects, including opioid dependence and exacerbation of symptoms. Moving forward, a multidisciplinary approach that addresses both gastrointestinal symptoms and pain management is warranted to improve outcomes and quality of life for patients with IBS.
Disclosures:
Evelyn Calderon Martinez indicated no relevant financial relationships.
Lidia Cardelle indicated no relevant financial relationships.
Adalberto Guzman indicated no relevant financial relationships.
Diana Gavilanes indicated no relevant financial relationships.
Shane Tripp indicated no relevant financial relationships.
Julianna Kinsolving indicated no relevant financial relationships.
Mauricio Alvarado indicated no relevant financial relationships.
Rodrigo Villata indicated no relevant financial relationships.
Anas Atras indicated no relevant financial relationships.
Evelyn Calderon Martinez, MD1, Lidia Cardelle, MS2, Adalberto Guzman, MD3, Diana Gavilanes, MD1, Shane Tripp, MS2, Julianna Kinsolving, MS2, Mauricio Alvarado, MD4, Rodrigo Villata, MD5, Anas Atras, MD1. P0614 - The Burden of Pain: High Rates of Opioid and Non-Opioid Analgesic Prescription in Patients With Irritable Bowel Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
