Sunday Poster Session
Category: Functional Bowel Disease
P0624 - GI-specific Anxiety, Not Generalized Anxiety or Depression, Linked to ARFID in Chronic Constipation
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Akua Nuako, MD
Massachusetts General Hospital
Boston, MA
Presenting Author(s)
Akua Nuako, MD1, Micaela Atkins, MD1, Sophie Abber, MS2, Victoria Beck, BA3, Jenna Clukey, BA3, Braden Kuo, MD, MSc, FACG3, Kyle Staller, MD, MPH3, Helen Burton-Murray, PhD3
1Massachusetts General Hospital, Boston, MA; 2Florida State University, Tallahassee, FL; 3Center for Neurointestinal Health, Massachusetts General Hospital, Boston, MA
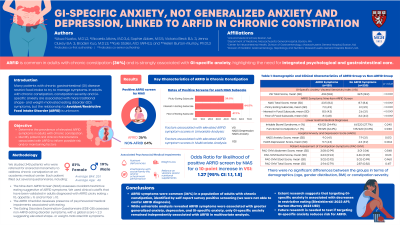
Introduction: Many patients with chronic gastrointestinal (GI) disease restrict food intake to manage symptoms. In adults with chronic constipation, constipation severity and GI-specific anxiety are associated with more traditional shape- and weight-motivated eating disorder (ED) symptoms, but the relationship to avoidant/restrictive food intake disorder (ARFID) is unknown. We aimed to (1) determine ARFID prevalence using a self-report survey and (2) identify possible risk/maintenance factors of ARFID in adults with chronic constipation.
Methods: We included 526 consecutive patients (80% female, mBMI=25, age 18-91) referred for anorectal manometry for chronic constipation at an academic medical center. Patients completed measures to assess ARFID symptoms using the Nine-Item ARFID Screen (NIAS) with a psychosocial/medical impairment checklist based on DSM-5 ARFID criteria, 8-item Eating Disorders Examination-Questionnaire (EDE-Q8) for other EDs, Hospital Anxiety and Depression Scale (HADS), Visceral Sensitivity Index (VSI) for GI-specific anxiety, and Patient Assessment of Constipation Symptoms (PAC-SYM) for symptom severity. We compared those with a negative screen on the NIAS to those with both a positive screen on at least one NIAS subscale and a negative screen for other ED symptoms (EDE-Q8 < 2.3).
Results: 179 (34%) patients screened positive for ARFID, 70 of whom also screened positive for another ED, leaving 109 (21%) in our analyzable ARFID group who had both a positive NIAS screen and a negative screen for other EDs (Table 1). Compared to those with a negative ARFID screen, those in our ARFID group had significantly more nutrition-related impairments. Groups did not differ in GI diagnoses, constipation symptom severity, generalized anxiety, or depression. On both univariate and multivariate analysis, lower BMI (OR=0.9; 95%CI=0.9-1.0) and higher GI-specific anxiety (OR=1.4 for every 10-point increase in VSI score; 95%CI=1.2-1.6) were significantly associated with a higher likelihood of being in the ARFID group.
Discussion: Screening positively on the NIAS for ARFID is common in patients with chronic constipation without other EDs (in 21%) and is associated with higher GI-specific anxiety, but not generalized anxiety, depression, or constipation severity. These findings suggest that GI-specific anxiety may be a convergent psychological risk/maintaining factor of ARFID in adults with chronic constipation, but future longitudinal research is needed.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Akua Nuako, MD1, Micaela Atkins, MD1, Sophie Abber, MS2, Victoria Beck, BA3, Jenna Clukey, BA3, Braden Kuo, MD, MSc, FACG3, Kyle Staller, MD, MPH3, Helen Burton-Murray, PhD3. P0624 - GI-specific Anxiety, Not Generalized Anxiety or Depression, Linked to ARFID in Chronic Constipation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Massachusetts General Hospital, Boston, MA; 2Florida State University, Tallahassee, FL; 3Center for Neurointestinal Health, Massachusetts General Hospital, Boston, MA
Introduction: Many patients with chronic gastrointestinal (GI) disease restrict food intake to manage symptoms. In adults with chronic constipation, constipation severity and GI-specific anxiety are associated with more traditional shape- and weight-motivated eating disorder (ED) symptoms, but the relationship to avoidant/restrictive food intake disorder (ARFID) is unknown. We aimed to (1) determine ARFID prevalence using a self-report survey and (2) identify possible risk/maintenance factors of ARFID in adults with chronic constipation.
Methods: We included 526 consecutive patients (80% female, mBMI=25, age 18-91) referred for anorectal manometry for chronic constipation at an academic medical center. Patients completed measures to assess ARFID symptoms using the Nine-Item ARFID Screen (NIAS) with a psychosocial/medical impairment checklist based on DSM-5 ARFID criteria, 8-item Eating Disorders Examination-Questionnaire (EDE-Q8) for other EDs, Hospital Anxiety and Depression Scale (HADS), Visceral Sensitivity Index (VSI) for GI-specific anxiety, and Patient Assessment of Constipation Symptoms (PAC-SYM) for symptom severity. We compared those with a negative screen on the NIAS to those with both a positive screen on at least one NIAS subscale and a negative screen for other ED symptoms (EDE-Q8 < 2.3).
Results: 179 (34%) patients screened positive for ARFID, 70 of whom also screened positive for another ED, leaving 109 (21%) in our analyzable ARFID group who had both a positive NIAS screen and a negative screen for other EDs (Table 1). Compared to those with a negative ARFID screen, those in our ARFID group had significantly more nutrition-related impairments. Groups did not differ in GI diagnoses, constipation symptom severity, generalized anxiety, or depression. On both univariate and multivariate analysis, lower BMI (OR=0.9; 95%CI=0.9-1.0) and higher GI-specific anxiety (OR=1.4 for every 10-point increase in VSI score; 95%CI=1.2-1.6) were significantly associated with a higher likelihood of being in the ARFID group.
Discussion: Screening positively on the NIAS for ARFID is common in patients with chronic constipation without other EDs (in 21%) and is associated with higher GI-specific anxiety, but not generalized anxiety, depression, or constipation severity. These findings suggest that GI-specific anxiety may be a convergent psychological risk/maintaining factor of ARFID in adults with chronic constipation, but future longitudinal research is needed.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Akua Nuako indicated no relevant financial relationships.
Micaela Atkins indicated no relevant financial relationships.
Sophie Abber indicated no relevant financial relationships.
Victoria Beck indicated no relevant financial relationships.
Jenna Clukey indicated no relevant financial relationships.
Braden Kuo: ATMO – Consultant, Grant/Research Support. Phathom – Consultant. Takeda – Advisory Committee/Board Member, Grant/Research Support.
Kyle Staller: Anji Pharmaceuticals – Consultant. Ardelyx – Consultant, Grant/Research Support. GI Supply – Consultant. Mahana Therapeutics – Consultant. Restalsis Health – Consultant, Grant/Research Support. Salix – Consultant.
Helen Burton-Murray indicated no relevant financial relationships.
Akua Nuako, MD1, Micaela Atkins, MD1, Sophie Abber, MS2, Victoria Beck, BA3, Jenna Clukey, BA3, Braden Kuo, MD, MSc, FACG3, Kyle Staller, MD, MPH3, Helen Burton-Murray, PhD3. P0624 - GI-specific Anxiety, Not Generalized Anxiety or Depression, Linked to ARFID in Chronic Constipation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

