Sunday Poster Session
Category: Esophagus
P0543 - Acute Esophageal Necrosis as a Result of Intraoperative Anesthesia
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- NS
Navjot Singh, MD
Inspira Health
Glassboro, NJ
Presenting Author(s)
Navjot Singh, MD1, Charles Sonaliya, MD2, Vincent Maiorino, DO3, Mahum Sami, DO4, Ashish Chawla, MD3, Christie Mannino, MD3
1Inspira Health, Glassboro, NJ; 2Smt. NHL Municipal Medical College, Vineland, NJ; 3Inspira Health, Vineland, NJ; 4Inspira Health Network, Glassboro, NJ
Introduction: Acute esophageal necrosis (AEN), also known as Gurvits syndrome, is a rare but critical cause of upper gastrointestinal bleeding, presenting as hematemesis or melena with an estimated prevalence of 0.01-0.28%. The exact cause remains unclear, but likely is multifactorial including ischemic injury, corrosive injury from stomach acid, and impaired mucosal barrier function. These factors are commonly seen in critically ill and malnourished patients.
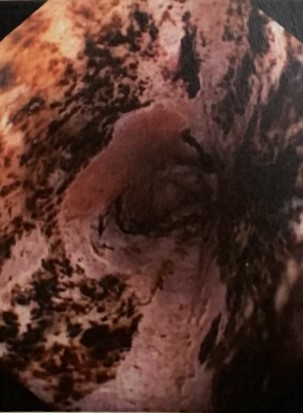
Case Description/Methods: We present a case of a 85-year-old gentleman with a history of hypertension, chronic kidney disease, and hyperlipidemia who underwent surgery for a fractured hip. During surgery, he experienced coffee-ground emesis, prompting an urgent bedside esophagogastroduodenoscopy (EGD). The EGD revealed esophagitis in the middle and lower esophagus, along with a concerning 6 cm segment of salmon-colored mucosa suggestive of Barrett’s esophagus. Biopsies were taken. Additionally, a circumferential black discoloration spanning 7-10 cm of the esophagus, consistent with necrosis, was observed. The stomach and duodenum appeared normal with no active bleeding. Biopsy results confirmed acute and chronic inflammation with necrosis, but no tumor cells were identified. Based on clinical presentation, EGD findings, and biopsies, AEN was diagnosed. Further investigation revealed a transient episode of hypotension following administration of anesthesia, potentially contributing to the esophageal insult.Treatment included twice daily proton pump inhibitors (PPIs) and sucralfate. Outpatient gastroenterology recommended continued PPI therapy and did not deem a repeat endoscopy necessary at this time. No further complications or development of sequelae were reported.
Discussion: This case underscores the importance of including AEN in the differential diagnosis for upper gastrointestinal bleeding in critically ill patients. Prompt recognition and management of the underlying causes are essential. This may involve correcting shock with appropriate resuscitation, implementing nil per os status, and suppressing gastric acid production with PPIs. Esophageal perforation is a potential acute complication, while chronic complications include stricture formation and tracheoesophageal fistulas.
Disclosures:
Navjot Singh, MD1, Charles Sonaliya, MD2, Vincent Maiorino, DO3, Mahum Sami, DO4, Ashish Chawla, MD3, Christie Mannino, MD3. P0543 - Acute Esophageal Necrosis as a Result of Intraoperative Anesthesia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Inspira Health, Glassboro, NJ; 2Smt. NHL Municipal Medical College, Vineland, NJ; 3Inspira Health, Vineland, NJ; 4Inspira Health Network, Glassboro, NJ
Introduction: Acute esophageal necrosis (AEN), also known as Gurvits syndrome, is a rare but critical cause of upper gastrointestinal bleeding, presenting as hematemesis or melena with an estimated prevalence of 0.01-0.28%. The exact cause remains unclear, but likely is multifactorial including ischemic injury, corrosive injury from stomach acid, and impaired mucosal barrier function. These factors are commonly seen in critically ill and malnourished patients.
Case Description/Methods: We present a case of a 85-year-old gentleman with a history of hypertension, chronic kidney disease, and hyperlipidemia who underwent surgery for a fractured hip. During surgery, he experienced coffee-ground emesis, prompting an urgent bedside esophagogastroduodenoscopy (EGD). The EGD revealed esophagitis in the middle and lower esophagus, along with a concerning 6 cm segment of salmon-colored mucosa suggestive of Barrett’s esophagus. Biopsies were taken. Additionally, a circumferential black discoloration spanning 7-10 cm of the esophagus, consistent with necrosis, was observed. The stomach and duodenum appeared normal with no active bleeding. Biopsy results confirmed acute and chronic inflammation with necrosis, but no tumor cells were identified. Based on clinical presentation, EGD findings, and biopsies, AEN was diagnosed. Further investigation revealed a transient episode of hypotension following administration of anesthesia, potentially contributing to the esophageal insult.Treatment included twice daily proton pump inhibitors (PPIs) and sucralfate. Outpatient gastroenterology recommended continued PPI therapy and did not deem a repeat endoscopy necessary at this time. No further complications or development of sequelae were reported.
Discussion: This case underscores the importance of including AEN in the differential diagnosis for upper gastrointestinal bleeding in critically ill patients. Prompt recognition and management of the underlying causes are essential. This may involve correcting shock with appropriate resuscitation, implementing nil per os status, and suppressing gastric acid production with PPIs. Esophageal perforation is a potential acute complication, while chronic complications include stricture formation and tracheoesophageal fistulas.
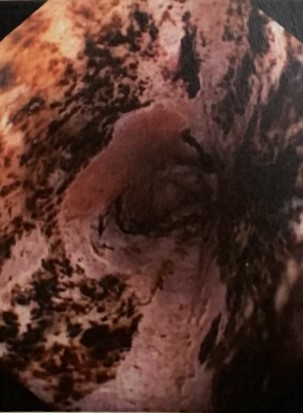
Figure: Circumferential black discoloration of the esophagus
Disclosures:
Navjot Singh indicated no relevant financial relationships.
Charles Sonaliya indicated no relevant financial relationships.
Vincent Maiorino indicated no relevant financial relationships.
Mahum Sami indicated no relevant financial relationships.
Ashish Chawla indicated no relevant financial relationships.
Christie Mannino indicated no relevant financial relationships.
Navjot Singh, MD1, Charles Sonaliya, MD2, Vincent Maiorino, DO3, Mahum Sami, DO4, Ashish Chawla, MD3, Christie Mannino, MD3. P0543 - Acute Esophageal Necrosis as a Result of Intraoperative Anesthesia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
