Sunday Poster Session
Category: Esophagus
P0546 - Atrioesophageal Fistula Following Catheter Ablation for Atrial Fibrillation
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- NO
Nazli Begum Ozturk, MD
Corewell Health William Beaumont University Hospital
Royal Oak, MI
Presenting Author(s)
Nazli Begum Ozturk, MD1, Ela Ahmad, MD2, Rabin Neupane, MD1, Fadi Odish, MD2
1Corewell Health William Beaumont University Hospital, Royal Oak, MI; 2Beaumont Health, Royal Oak, MI
Introduction: Due to the proximity of left atrium, esophagus is particularly prone to thermal injury during ablation for atrial arrhythmias. Although extremely rare, esophageal injuries such as ulceration or atrioesophageal fistula (AEF) have been reported after catheter ablation, occurring in < 1% of cases. In this case, we describe a patient with AEF presenting with hemorrhagic shock.
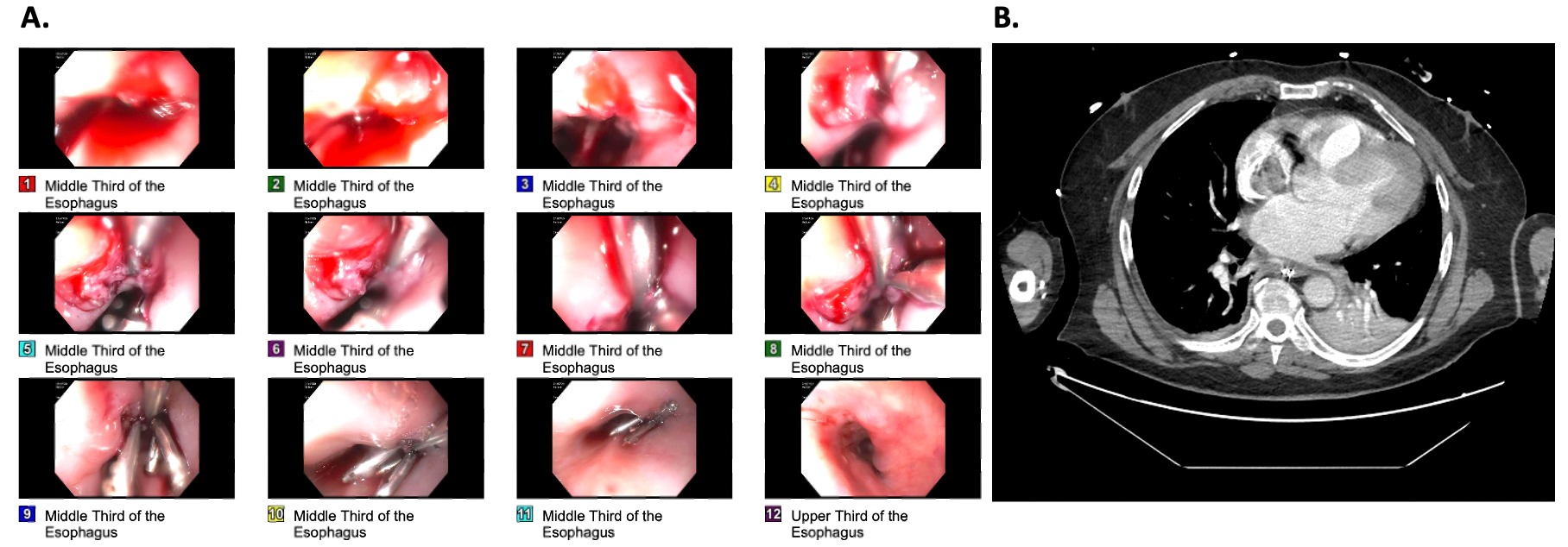
Case Description/Methods: A 67-year-old male with persistent atrial fibrillation and hypertension to the emergency department (ED) with one day history of melena and shortness of breath. Remarkably, he underwent pulmonary vein isolation (PVI) with radiofrequency ablation for atrial fibrillation and cavotricuspid ablation for separate and distinct atrial flutter ablation seven days prior. He was discharged home the next day with instructions to resume rivaroxaban. In the ED, his blood pressure was 140/90 mmHg and heart rate was 78 bpm. His last dose of rivaroxaban was the day prior. On examination he was diaphoretic. Laboratory workup revelated an acute decrease in hemoglobin to 10.8 g/dL from 13.3 g/dL. CT chest was remarkable for gastric wall distention. He had another episode of melena in ED and had hypotension (90/60 mmHg) and tachycardia (120 bpm). A repeat hemoglobin was at 8.5 g/dL. Intravenous fluids, proton pump inhibitor infusion, and 2 packed red blood cell transfusion were initiated. An urgent EGD was done with findings of active extravasation from esophageal ulcer (5-6 mm) at 35 cm from the incisors, and large blood clots in esophagus and stomach. Endoscopic treatment with epinephrine and 4 endoclips placement (Figure 1A) were done. Patient was transferred to the intensive care unit as he was requiring vasopressor support. His blood pressure has improved, and hemoglobin remained stable between 8-9 g/dL with no active bleeding, and discharged home on day six. Six days later he presented to the ED again with generalized weakness and a CT scan showed AEF, and the patient underwent emergent right thoracotomy and the repair of left AEF (Figure 1B). A repeat EGD done showing 2.4 cm esophageal leak and an esophageal stent and PEG tube was placed, which were removed in 4 weeks after another EGD and barium esophagogram.
Discussion: Esophageal injuries are rare after catheter ablation for atrial arrythmias. As the catheter is in the left atrium, the mucosa of the esophagus is farthest from the heat source, and the presence of mucosal erythema or ulceration is suggestive of a significant injury, as seen in our case.
Disclosures:
Nazli Begum Ozturk, MD1, Ela Ahmad, MD2, Rabin Neupane, MD1, Fadi Odish, MD2. P0546 - Atrioesophageal Fistula Following Catheter Ablation for Atrial Fibrillation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Corewell Health William Beaumont University Hospital, Royal Oak, MI; 2Beaumont Health, Royal Oak, MI
Introduction: Due to the proximity of left atrium, esophagus is particularly prone to thermal injury during ablation for atrial arrhythmias. Although extremely rare, esophageal injuries such as ulceration or atrioesophageal fistula (AEF) have been reported after catheter ablation, occurring in < 1% of cases. In this case, we describe a patient with AEF presenting with hemorrhagic shock.
Case Description/Methods: A 67-year-old male with persistent atrial fibrillation and hypertension to the emergency department (ED) with one day history of melena and shortness of breath. Remarkably, he underwent pulmonary vein isolation (PVI) with radiofrequency ablation for atrial fibrillation and cavotricuspid ablation for separate and distinct atrial flutter ablation seven days prior. He was discharged home the next day with instructions to resume rivaroxaban. In the ED, his blood pressure was 140/90 mmHg and heart rate was 78 bpm. His last dose of rivaroxaban was the day prior. On examination he was diaphoretic. Laboratory workup revelated an acute decrease in hemoglobin to 10.8 g/dL from 13.3 g/dL. CT chest was remarkable for gastric wall distention. He had another episode of melena in ED and had hypotension (90/60 mmHg) and tachycardia (120 bpm). A repeat hemoglobin was at 8.5 g/dL. Intravenous fluids, proton pump inhibitor infusion, and 2 packed red blood cell transfusion were initiated. An urgent EGD was done with findings of active extravasation from esophageal ulcer (5-6 mm) at 35 cm from the incisors, and large blood clots in esophagus and stomach. Endoscopic treatment with epinephrine and 4 endoclips placement (Figure 1A) were done. Patient was transferred to the intensive care unit as he was requiring vasopressor support. His blood pressure has improved, and hemoglobin remained stable between 8-9 g/dL with no active bleeding, and discharged home on day six. Six days later he presented to the ED again with generalized weakness and a CT scan showed AEF, and the patient underwent emergent right thoracotomy and the repair of left AEF (Figure 1B). A repeat EGD done showing 2.4 cm esophageal leak and an esophageal stent and PEG tube was placed, which were removed in 4 weeks after another EGD and barium esophagogram.
Discussion: Esophageal injuries are rare after catheter ablation for atrial arrythmias. As the catheter is in the left atrium, the mucosa of the esophagus is farthest from the heat source, and the presence of mucosal erythema or ulceration is suggestive of a significant injury, as seen in our case.
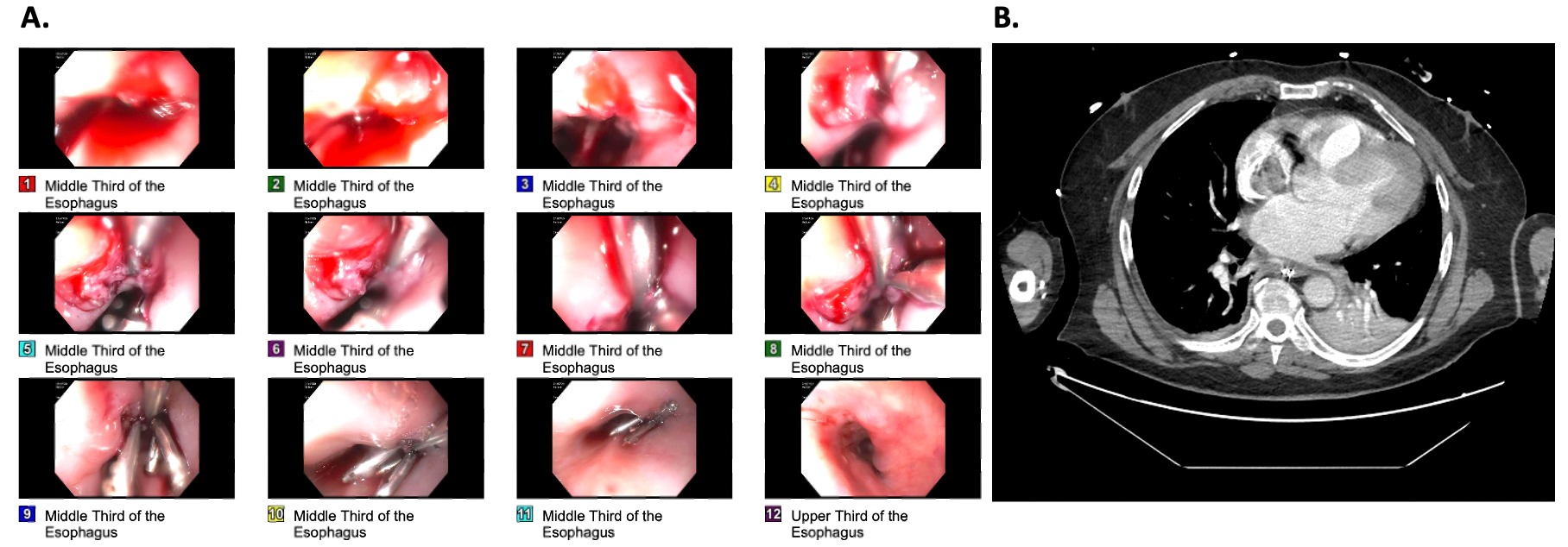
Figure: A: EGD with a cratered ulcer spurting blood at 35 cm from the incisors (5-6 mm in the largest dimension), treated with epinephrine and hemostatic clips. B: CT view of the atrioesophageal fistula.
Disclosures:
Nazli Begum Ozturk indicated no relevant financial relationships.
Ela Ahmad indicated no relevant financial relationships.
Rabin Neupane indicated no relevant financial relationships.
Fadi Odish indicated no relevant financial relationships.
Nazli Begum Ozturk, MD1, Ela Ahmad, MD2, Rabin Neupane, MD1, Fadi Odish, MD2. P0546 - Atrioesophageal Fistula Following Catheter Ablation for Atrial Fibrillation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
