Sunday Poster Session
Category: Esophagus
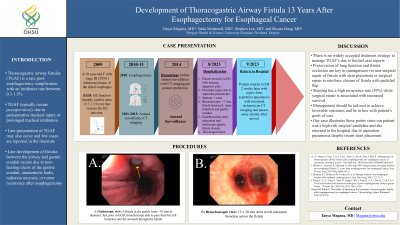
P0551 - A Case of Thoracogastric Airway Fistula: A Serious Complication 13 Years After Esophagectomy for Esophageal Cancer
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Tanya Magana, MD
Oregon Health & Science University
Portland, OR
Presenting Author(s)
Award: Presidential Poster Award
Tanya Magana, MD, Nada Mohamed, MD, Stephen Lee, MD, Shyam Dang, MD
Oregon Health & Science University, Portland, OR
Introduction: Thoracogastric airway fistulas (TGAF) is a rare post-esophagectomy complication with an incidence rate between 0.3-1.5%. TGAF typically occurs postoperatively due to perioperative tracheal injury or prolonged tracheal intubation, which can result in recurrent pneumonia and respiratory failure. However, late presentation of TGAF may also occur, with only a few cases reported in the literature.
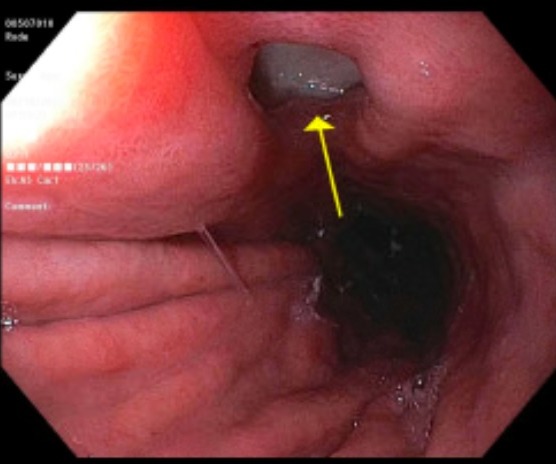
Case Description/Methods: A 78-year-old female presented with stage III (T3N1) adenocarcinoma of the distal esophagus in 2009 and underwent an esophagectomy in 2010. Annual computed tomography (CT) surveillance from 2011-2013 revealed no recurrence and she opted to discontinue further monitoring. In 2023, she presented with severe, burning epigastric pain, odynophagia, and shortness of breath for one day. CT chest showed a rounded area of density along the right medial base and bronchi. Due to suspected aspiration pneumonia, patient was started on antibiotics. Barium swallow study showed mild aspiration followed by an esophagram with large volume aspiration, which prompted early termination. Patient developed new oxygen requirements, worsening leukocytosis, and yeast growth in sputum culture. Bronchoscopy revealed a 7 mm fistula between the left main bronchus and gastric conduit. Upper endoscopy also revealed ulceration with biopsy confirming intestinal metaplasia. Treatment with endobronchial stent placement and endoscopic gastric fistula closure was chosen, but she returned two weeks later due to sepsis from aspiration pneumonia with intestinal ischemia and she passed away shortly after.
Discussion: Late development of fistulas between the airway and gastric conduit occurs due to non-healing ulcers of the gastric conduit, anastomotic leaks, radiation necrosis, or tumor recurrence after esophagectomy. Management is challenging and there is no widely accepted treatment strategy due to limited case reports. However, preservation of lung function and fistula occlusion is crucial in management. This involves either non-surgical stent placement or surgical repair to reinforce closure of the fistula with pedicled flap. Stenting has a high recurrence rate (39%), while surgical repair is associated with increased survival. Patient presentations vary, precluding a uniform treatment approach. Therefore, management should be tailored to optimize outcomes and align with patients’ goals of care. Our case illustrates this, as our patient was a high-risk surgical candidate who developed post-stent aspiration pneumonia.
Disclosures:
Tanya Magana, MD, Nada Mohamed, MD, Stephen Lee, MD, Shyam Dang, MD. P0551 - A Case of Thoracogastric Airway Fistula: A Serious Complication 13 Years After Esophagectomy for Esophageal Cancer, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Tanya Magana, MD, Nada Mohamed, MD, Stephen Lee, MD, Shyam Dang, MD
Oregon Health & Science University, Portland, OR
Introduction: Thoracogastric airway fistulas (TGAF) is a rare post-esophagectomy complication with an incidence rate between 0.3-1.5%. TGAF typically occurs postoperatively due to perioperative tracheal injury or prolonged tracheal intubation, which can result in recurrent pneumonia and respiratory failure. However, late presentation of TGAF may also occur, with only a few cases reported in the literature.
Case Description/Methods: A 78-year-old female presented with stage III (T3N1) adenocarcinoma of the distal esophagus in 2009 and underwent an esophagectomy in 2010. Annual computed tomography (CT) surveillance from 2011-2013 revealed no recurrence and she opted to discontinue further monitoring. In 2023, she presented with severe, burning epigastric pain, odynophagia, and shortness of breath for one day. CT chest showed a rounded area of density along the right medial base and bronchi. Due to suspected aspiration pneumonia, patient was started on antibiotics. Barium swallow study showed mild aspiration followed by an esophagram with large volume aspiration, which prompted early termination. Patient developed new oxygen requirements, worsening leukocytosis, and yeast growth in sputum culture. Bronchoscopy revealed a 7 mm fistula between the left main bronchus and gastric conduit. Upper endoscopy also revealed ulceration with biopsy confirming intestinal metaplasia. Treatment with endobronchial stent placement and endoscopic gastric fistula closure was chosen, but she returned two weeks later due to sepsis from aspiration pneumonia with intestinal ischemia and she passed away shortly after.
Discussion: Late development of fistulas between the airway and gastric conduit occurs due to non-healing ulcers of the gastric conduit, anastomotic leaks, radiation necrosis, or tumor recurrence after esophagectomy. Management is challenging and there is no widely accepted treatment strategy due to limited case reports. However, preservation of lung function and fistula occlusion is crucial in management. This involves either non-surgical stent placement or surgical repair to reinforce closure of the fistula with pedicled flap. Stenting has a high recurrence rate (39%), while surgical repair is associated with increased survival. Patient presentations vary, precluding a uniform treatment approach. Therefore, management should be tailored to optimize outcomes and align with patients’ goals of care. Our case illustrates this, as our patient was a high-risk surgical candidate who developed post-stent aspiration pneumonia.
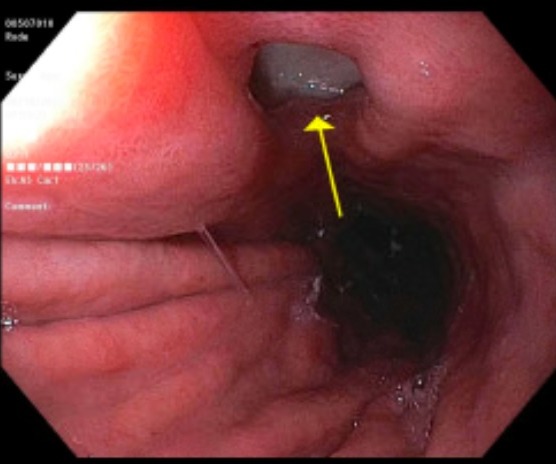
Figure: Endoscopic view: evidence of esophagectomy with gastric pull up. A fistula is visualized in the gastric body approximately 10 mm in diameter. The fistula was confirmed just prior to upper endoscopy by bronchoscopy, which allowed for passage of the bronchoscope from patient's left bronchus into the stomach through the fistula.
Disclosures:
Tanya Magana indicated no relevant financial relationships.
Nada Mohamed indicated no relevant financial relationships.
Stephen Lee indicated no relevant financial relationships.
Shyam Dang indicated no relevant financial relationships.
Tanya Magana, MD, Nada Mohamed, MD, Stephen Lee, MD, Shyam Dang, MD. P0551 - A Case of Thoracogastric Airway Fistula: A Serious Complication 13 Years After Esophagectomy for Esophageal Cancer, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

