Sunday Poster Session
Category: Esophagus
P0552 - Esophageal Histoplasmosis: A Rare Cause of Odynophagia
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Shruti Kulkarni, MD
University of South Florida
Tampa, FL
Presenting Author(s)
Award: Presidential Poster Award
Shruti Kulkarni, MD1, Susan Jacob, MD1, David Metter, MD2, Jonathan Hilal, MD1
1University of South Florida, Tampa, FL; 2Tampa General Hospital / University of South Florida, Tampa, FL
Introduction: Histoplasmosis is an opportunistic infection occurring in immunocompromised patients. In the GI tract, the terminal ileum and colon are most often affected leading to diarrhea and abdominal pain. The disease can also affect the esophagus, though primary esophageal involvement is rare.
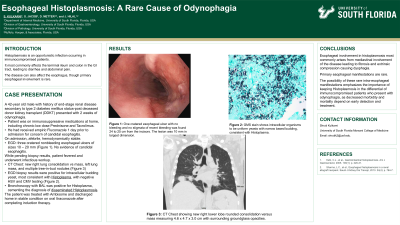
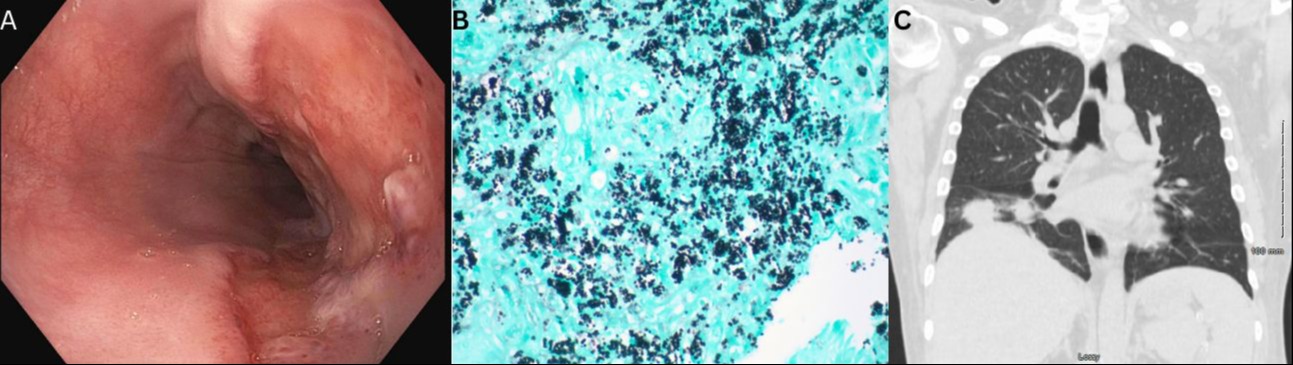
Case Description/Methods: This is a case of a 42 year-old male with history of end-stage renal disease secondary to type 2 diabetes mellitus status post deceased donor kidney transplant who presented with 2 weeks of odynophagia. The patient’s home medications included chronic low dose prednisone, tacrolimus, and valganciclovir. Of note, the patient was prescribed Fluconazole for empiric treatment of esophageal candidiasis by his primary care physician, which he took the day prior to admission. On admission, the patient was afebrile and hemodynamically stable. EGD showed three cratered nonbleeding esophageal ulcers of sizes 10 – 20 mm, but no evidence of candidal esophagitis (Figure 1A). Biopsies were taken for histology to assess for infectious viral etiologies. He fevered and underwent infectious workup including CT chest which showed a new right lung consolidation vs mass, left lung mass, and multiple tree-in-bud nodules (Figure 1C). EGD pathology resulted positive for intracellular budding yeast, most consistent with Histoplasma, with negative HSV and CMV testing (Figure 1B). Bronchoscopy with BAL was performed from which cytology showed fungal organisms and cultures grew Histoplasma, cementing the diagnosis of disseminated Histoplasmosis. He started treatment with Ambisome and after completing induction therapy, was discharged home on oral Itraconazole.
Discussion: Esophageal involvement in histoplasmosis most commonly arises from mediastinal involvement of the disease leading to fibrosis and extrinsic compression causing dysphagia. Primary esophageal manifestations are rare[1]. Some case studies have noted primary esophageal histoplasmosis presenting as either ulcerations or polyps [2]. The possibility of these rare intra-esophageal manifestations emphasizes the importance of keeping Histoplasmosis in the differential of immunocompromised patients who present with odynophagia, as decreased morbidity and mortality depend on early detection and treatment.
1. Kahi, C.J., et al., Gastrointestinal histoplasmosis. Am J Gastroenterol, 2005. 100(1): p. 220-31.
2. Sharma, L.C., et al., Esophageal histoplasmosis in a renal allograft recipient. Saudi J Kidney Dis Transpl, 2013. 24(4): p. 764-7.
Disclosures:
Shruti Kulkarni, MD1, Susan Jacob, MD1, David Metter, MD2, Jonathan Hilal, MD1. P0552 - Esophageal Histoplasmosis: A Rare Cause of Odynophagia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Shruti Kulkarni, MD1, Susan Jacob, MD1, David Metter, MD2, Jonathan Hilal, MD1
1University of South Florida, Tampa, FL; 2Tampa General Hospital / University of South Florida, Tampa, FL
Introduction: Histoplasmosis is an opportunistic infection occurring in immunocompromised patients. In the GI tract, the terminal ileum and colon are most often affected leading to diarrhea and abdominal pain. The disease can also affect the esophagus, though primary esophageal involvement is rare.
Case Description/Methods: This is a case of a 42 year-old male with history of end-stage renal disease secondary to type 2 diabetes mellitus status post deceased donor kidney transplant who presented with 2 weeks of odynophagia. The patient’s home medications included chronic low dose prednisone, tacrolimus, and valganciclovir. Of note, the patient was prescribed Fluconazole for empiric treatment of esophageal candidiasis by his primary care physician, which he took the day prior to admission. On admission, the patient was afebrile and hemodynamically stable. EGD showed three cratered nonbleeding esophageal ulcers of sizes 10 – 20 mm, but no evidence of candidal esophagitis (Figure 1A). Biopsies were taken for histology to assess for infectious viral etiologies. He fevered and underwent infectious workup including CT chest which showed a new right lung consolidation vs mass, left lung mass, and multiple tree-in-bud nodules (Figure 1C). EGD pathology resulted positive for intracellular budding yeast, most consistent with Histoplasma, with negative HSV and CMV testing (Figure 1B). Bronchoscopy with BAL was performed from which cytology showed fungal organisms and cultures grew Histoplasma, cementing the diagnosis of disseminated Histoplasmosis. He started treatment with Ambisome and after completing induction therapy, was discharged home on oral Itraconazole.
Discussion: Esophageal involvement in histoplasmosis most commonly arises from mediastinal involvement of the disease leading to fibrosis and extrinsic compression causing dysphagia. Primary esophageal manifestations are rare[1]. Some case studies have noted primary esophageal histoplasmosis presenting as either ulcerations or polyps [2]. The possibility of these rare intra-esophageal manifestations emphasizes the importance of keeping Histoplasmosis in the differential of immunocompromised patients who present with odynophagia, as decreased morbidity and mortality depend on early detection and treatment.
1. Kahi, C.J., et al., Gastrointestinal histoplasmosis. Am J Gastroenterol, 2005. 100(1): p. 220-31.
2. Sharma, L.C., et al., Esophageal histoplasmosis in a renal allograft recipient. Saudi J Kidney Dis Transpl, 2013. 24(4): p. 764-7.
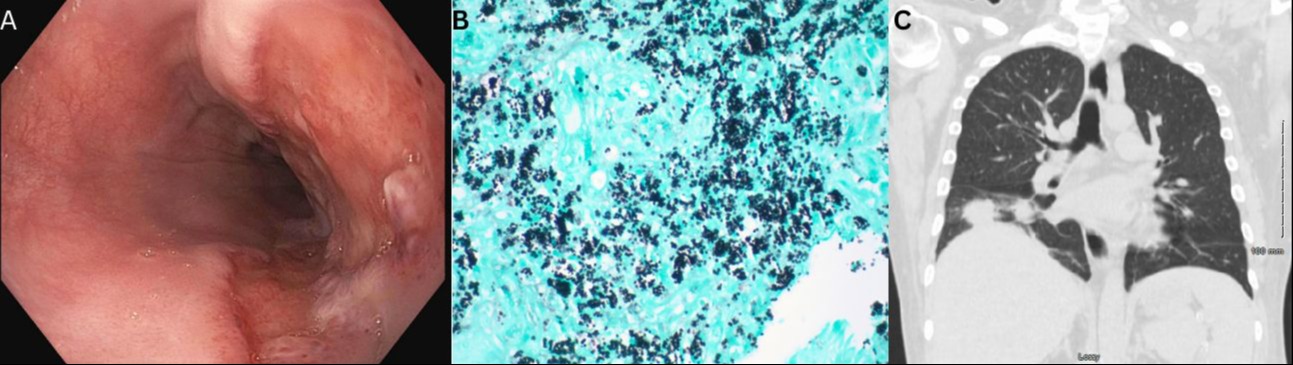
Figure: Image A: One cratered esophageal ulcer with no bleeding and no stigmata of recent bleeding was found 24 to 25 cm from the incisors. The lesion was 10 mm in largest dimension.
Image B: GMS stain shows intracellular organisms to be uniform yeasts with narrow based budding, consistent with Histoplasma.
Image C: CT scan of chest showing new right lower lobe development of rounded consolidation versus mass within the right lower lobe measuring 4.6 x 4.7 x 3.0 cm with surrounding groundglass opacities.
Image B: GMS stain shows intracellular organisms to be uniform yeasts with narrow based budding, consistent with Histoplasma.
Image C: CT scan of chest showing new right lower lobe development of rounded consolidation versus mass within the right lower lobe measuring 4.6 x 4.7 x 3.0 cm with surrounding groundglass opacities.
Disclosures:
Shruti Kulkarni indicated no relevant financial relationships.
Susan Jacob indicated no relevant financial relationships.
David Metter indicated no relevant financial relationships.
Jonathan Hilal indicated no relevant financial relationships.
Shruti Kulkarni, MD1, Susan Jacob, MD1, David Metter, MD2, Jonathan Hilal, MD1. P0552 - Esophageal Histoplasmosis: A Rare Cause of Odynophagia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

