Sunday Poster Session
Category: Esophagus
P0553 - Complete Esophageal Obstruction With Endoscopic Rendezvous
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Michael Bebawy, DO
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Michael Bebawy, DO1, Kranthi Mandava, MD1, Mohamed Ismail, DO1, Menna-Allah Elaskandrany, DO2, Shivani Patel, MD1, Ahmed Al-Khazraji, MD1, Kaveh Hajifathalian, MD1
1Rutgers New Jersey Medical School, Newark, NJ; 2Lenox Hill Hospital, Northwell Health, Astoria, NY
Introduction: Complete esophageal obstruction is a rare complication after head and neck cancer treated with chemoradiation. Patients will commonly present with dysphagia which can significantly impact a patient's quality of life. Traditionally, these strictures have been treated with open surgical procedures. However, recent advancements in endoscopic procedures have introduced minimally invasive techniques that have led to faster recovery and reduced risks of complications. We present a case of a patient whose complete esophageal obstruction was alleviated by the timely utilization of the esophageal rendezvous procedure.
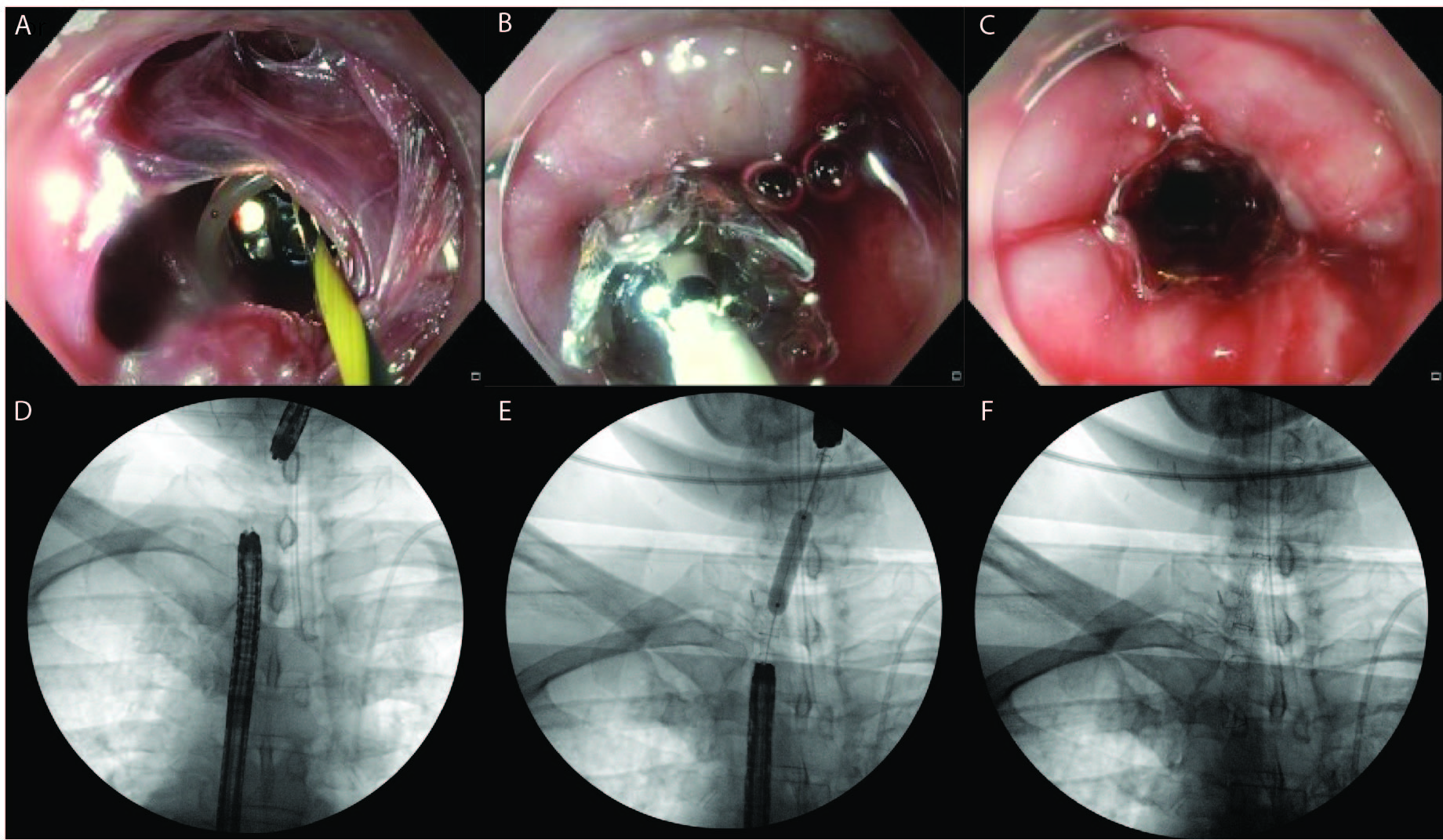
Case Description/Methods: A 55 year old year old male with a past medical history of anaplastic thyroid cancer (pT3AN1BMx) status post total thyroidectomy and chemoradiation presented with dysphagia. The patient had reported an inability to swallow saliva, needing to constantly spit up, severely disturbing his normal daily life. A complete upper esophageal obstruction was confirmed and after discussion of risks and benefits, endoscopic rendezvous was offered.
First the PEG tube was removed and the PEG insertion site was dilated with a Savary Dilator. The Endoscope was passed through the PEG site and a guidewire inserted into the scope. A second endoscope was passed into the proximal esophagus. Approximately a 3cm area of esophageal scarring was noted using fluoroscopy and unable to rendezvous. A needle knife was used to dissect through esophageal scarring and a wire was threaded through the area until visualized. Forceps were then used to advance the guidewire through the mouth. An esophageal stent 8 x 8 was placed along the proximal esophagus using the antegrade endoscope and dilated using Hurricane. A second esophageal stent 10x8 was placed with overlap of the proximal esophageal stent and visualized with fluoroscopy. Finally the PEG tube was replaced. The procedure was successful and the patient was scheduled for follow up for serial dilations to maintain luminal patency.
Discussion: Endoscopic antegrade-retrograde rendezvous, while a very technical and difficult procedure offers a safe and viable alternative to high risk surgical approaches or a blind antegrade approach. Many patients have significant improvement in their clinical symptoms such as swallowing, while some patients are able to become PEG tube independent. Further clinical research is required to better understand the frequency with which patients are able to tolerate PO and become PEG tube independent.
Disclosures:
Michael Bebawy, DO1, Kranthi Mandava, MD1, Mohamed Ismail, DO1, Menna-Allah Elaskandrany, DO2, Shivani Patel, MD1, Ahmed Al-Khazraji, MD1, Kaveh Hajifathalian, MD1. P0553 - Complete Esophageal Obstruction With Endoscopic Rendezvous, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Newark, NJ; 2Lenox Hill Hospital, Northwell Health, Astoria, NY
Introduction: Complete esophageal obstruction is a rare complication after head and neck cancer treated with chemoradiation. Patients will commonly present with dysphagia which can significantly impact a patient's quality of life. Traditionally, these strictures have been treated with open surgical procedures. However, recent advancements in endoscopic procedures have introduced minimally invasive techniques that have led to faster recovery and reduced risks of complications. We present a case of a patient whose complete esophageal obstruction was alleviated by the timely utilization of the esophageal rendezvous procedure.
Case Description/Methods: A 55 year old year old male with a past medical history of anaplastic thyroid cancer (pT3AN1BMx) status post total thyroidectomy and chemoradiation presented with dysphagia. The patient had reported an inability to swallow saliva, needing to constantly spit up, severely disturbing his normal daily life. A complete upper esophageal obstruction was confirmed and after discussion of risks and benefits, endoscopic rendezvous was offered.
First the PEG tube was removed and the PEG insertion site was dilated with a Savary Dilator. The Endoscope was passed through the PEG site and a guidewire inserted into the scope. A second endoscope was passed into the proximal esophagus. Approximately a 3cm area of esophageal scarring was noted using fluoroscopy and unable to rendezvous. A needle knife was used to dissect through esophageal scarring and a wire was threaded through the area until visualized. Forceps were then used to advance the guidewire through the mouth. An esophageal stent 8 x 8 was placed along the proximal esophagus using the antegrade endoscope and dilated using Hurricane. A second esophageal stent 10x8 was placed with overlap of the proximal esophageal stent and visualized with fluoroscopy. Finally the PEG tube was replaced. The procedure was successful and the patient was scheduled for follow up for serial dilations to maintain luminal patency.
Discussion: Endoscopic antegrade-retrograde rendezvous, while a very technical and difficult procedure offers a safe and viable alternative to high risk surgical approaches or a blind antegrade approach. Many patients have significant improvement in their clinical symptoms such as swallowing, while some patients are able to become PEG tube independent. Further clinical research is required to better understand the frequency with which patients are able to tolerate PO and become PEG tube independent.
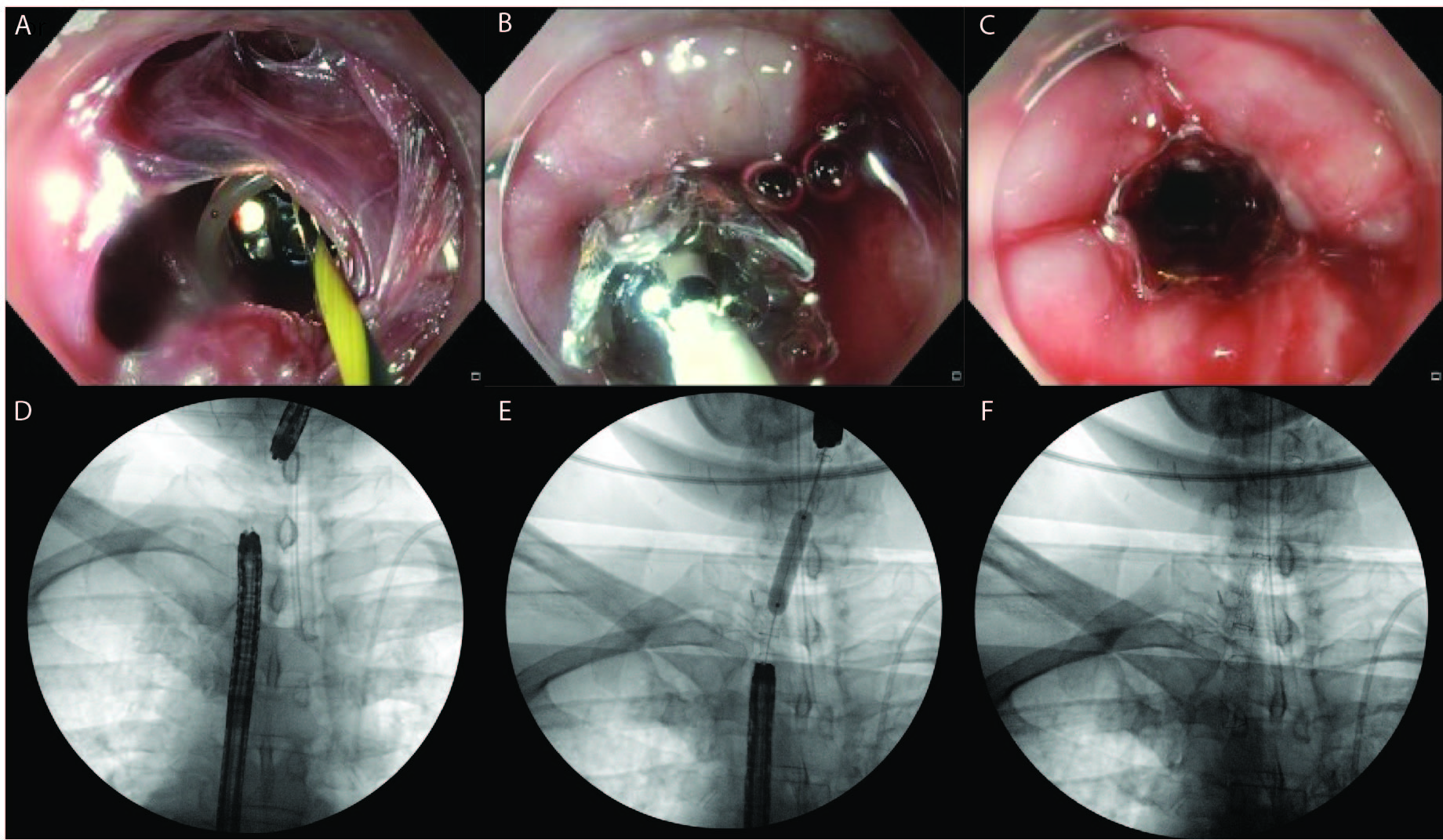
Figure: A - Endoscopic Rendezvous
B - Dilation of esophageal stent
C - Patent esophageal lumen after stenting
D - Incomplete Endoscopic Rendezvous
E - Dilation of esophageal stent
F - Patent esophageal lumen after stenting
B - Dilation of esophageal stent
C - Patent esophageal lumen after stenting
D - Incomplete Endoscopic Rendezvous
E - Dilation of esophageal stent
F - Patent esophageal lumen after stenting
Disclosures:
Michael Bebawy indicated no relevant financial relationships.
Kranthi Mandava indicated no relevant financial relationships.
Mohamed Ismail indicated no relevant financial relationships.
Menna-Allah Elaskandrany indicated no relevant financial relationships.
Shivani Patel indicated no relevant financial relationships.
Ahmed Al-Khazraji indicated no relevant financial relationships.
Kaveh Hajifathalian indicated no relevant financial relationships.
Michael Bebawy, DO1, Kranthi Mandava, MD1, Mohamed Ismail, DO1, Menna-Allah Elaskandrany, DO2, Shivani Patel, MD1, Ahmed Al-Khazraji, MD1, Kaveh Hajifathalian, MD1. P0553 - Complete Esophageal Obstruction With Endoscopic Rendezvous, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
