Sunday Poster Session
Category: Endoscopy Video Forum
P0467 - Drowning in Food? Management of an Esophagojejunal Anastomotic Dehiscence through Endoluminal Vacuum Therapy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Kazi T. Haque, MD
University of Texas Health, McGovern Medical School
Pearland, TX
Presenting Author(s)
Kazi T. Haque, MD1, Nitish Mittal, MD2, Iyad Al-bustami, MD, MPH(c)3, Ingrid Schwartz, MD4, Jeffrey H.. Lee, MD, MPH, FACG4, Emmanuel Coronel, MD4
1University of Texas Health, McGovern Medical School, Pearland, TX; 2University of Texas Health, McGovern Medical School, Houston, TX; 3Brooklyn Hospital Center, Houston, TX; 4MD Anderson Cancer Center, Houston, TX
Introduction: Esophagojejunal (EJ) anastomosis after a gastrectomy is common, but one deadly complication is an anastomotic leak/dehiscence. We highlight a case of an EJ anastomosis leak managed by endoluminal vacuum therapy (EVT) with stent placement.
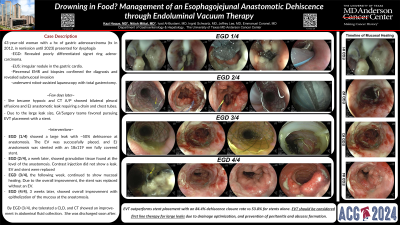
Case Description/Methods: A 43-year-old woman with gastric adenocarcinoma underwent total gastrectomy that was complicated by an EJ anastomotic leak. Treated for gastric cancer in 2012, she was in remission until 2023. Due to dysphagia, she underwent an esophagogastroduodenoscopy (EGD) with biopsies that revealed poorly differentiated signet ring adenocarcinoma. Endoscopic ultrasound later showed an irregular nodule in the gastric cardia. Piecemeal endoscopic mucosal resection and biopsies confirmed the diagnosis and revealed submucosal invasion with positive distal margins. She then underwent robot-assisted laparoscopy with total gastrectomy. A few days later, she became hypoxic with computed tomography chest/abdomen showed bilateral pleural effusions and EJ anastomotic leak requiring a percutaneous abdominal drain. An interdisciplinary discussion between gastroenterology and surgery favored pursuing EVT placement with a stent. EGD then showed a large fistula at the level of anastomosis with ~50% dehiscence. The EV was successfully placed, and EJ anastomosis was stented with an 18x119 mm fully covered stent. A week later, EGD showed granulation tissue found at the level of the anastomosis. Contrast injection did not show a leak. The EV and stent were replaced. Next week, EGD continued to show mucosal healing. Due to the overall improvement, the stent was replaced without EV placement. Afterwards, the patient tolerated a clear liquid diet, and computed tomography scan showed an improvement in abdominal fluid collection. Final EGD, 3 weeks later, showed overall improvement with epithelization of the mucosa at the anastomosis, and she was later discharged.
Discussion: 30-day mortality rate of patients with anastomotic leaks range from 17-35% compared to 2%-3% of patients without leaks. To provide a minimally invasive solution for anastomotic leaks, self-expanding stents acted as first line therapy before EVT. EVT outperforms stent placement with an 84.4% closure rate compared to 53.8% for stents. Advantages of EVT over stent therapy include providing optimal drainage of the wound preventing peritonitis and abscess formation as well as providing clear visualization of the wound cavity. Hence, our case sheds light on the relevance and utility of EVT with stents in EJ anastomotic leaks.
Disclosures:
Kazi T. Haque, MD1, Nitish Mittal, MD2, Iyad Al-bustami, MD, MPH(c)3, Ingrid Schwartz, MD4, Jeffrey H.. Lee, MD, MPH, FACG4, Emmanuel Coronel, MD4. P0467 - Drowning in Food? Management of an Esophagojejunal Anastomotic Dehiscence through Endoluminal Vacuum Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health, McGovern Medical School, Pearland, TX; 2University of Texas Health, McGovern Medical School, Houston, TX; 3Brooklyn Hospital Center, Houston, TX; 4MD Anderson Cancer Center, Houston, TX
Introduction: Esophagojejunal (EJ) anastomosis after a gastrectomy is common, but one deadly complication is an anastomotic leak/dehiscence. We highlight a case of an EJ anastomosis leak managed by endoluminal vacuum therapy (EVT) with stent placement.
Case Description/Methods: A 43-year-old woman with gastric adenocarcinoma underwent total gastrectomy that was complicated by an EJ anastomotic leak. Treated for gastric cancer in 2012, she was in remission until 2023. Due to dysphagia, she underwent an esophagogastroduodenoscopy (EGD) with biopsies that revealed poorly differentiated signet ring adenocarcinoma. Endoscopic ultrasound later showed an irregular nodule in the gastric cardia. Piecemeal endoscopic mucosal resection and biopsies confirmed the diagnosis and revealed submucosal invasion with positive distal margins. She then underwent robot-assisted laparoscopy with total gastrectomy. A few days later, she became hypoxic with computed tomography chest/abdomen showed bilateral pleural effusions and EJ anastomotic leak requiring a percutaneous abdominal drain. An interdisciplinary discussion between gastroenterology and surgery favored pursuing EVT placement with a stent. EGD then showed a large fistula at the level of anastomosis with ~50% dehiscence. The EV was successfully placed, and EJ anastomosis was stented with an 18x119 mm fully covered stent. A week later, EGD showed granulation tissue found at the level of the anastomosis. Contrast injection did not show a leak. The EV and stent were replaced. Next week, EGD continued to show mucosal healing. Due to the overall improvement, the stent was replaced without EV placement. Afterwards, the patient tolerated a clear liquid diet, and computed tomography scan showed an improvement in abdominal fluid collection. Final EGD, 3 weeks later, showed overall improvement with epithelization of the mucosa at the anastomosis, and she was later discharged.
Discussion: 30-day mortality rate of patients with anastomotic leaks range from 17-35% compared to 2%-3% of patients without leaks. To provide a minimally invasive solution for anastomotic leaks, self-expanding stents acted as first line therapy before EVT. EVT outperforms stent placement with an 84.4% closure rate compared to 53.8% for stents. Advantages of EVT over stent therapy include providing optimal drainage of the wound preventing peritonitis and abscess formation as well as providing clear visualization of the wound cavity. Hence, our case sheds light on the relevance and utility of EVT with stents in EJ anastomotic leaks.
Disclosures:
Kazi Haque indicated no relevant financial relationships.
Nitish Mittal indicated no relevant financial relationships.
Iyad Al-bustami indicated no relevant financial relationships.
Ingrid Schwartz indicated no relevant financial relationships.
Jeffrey Lee: Boston Scientific – Consultant. Pentax – Consultant.
Emmanuel Coronel indicated no relevant financial relationships.
Kazi T. Haque, MD1, Nitish Mittal, MD2, Iyad Al-bustami, MD, MPH(c)3, Ingrid Schwartz, MD4, Jeffrey H.. Lee, MD, MPH, FACG4, Emmanuel Coronel, MD4. P0467 - Drowning in Food? Management of an Esophagojejunal Anastomotic Dehiscence through Endoluminal Vacuum Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
