Sunday Poster Session
Category: Esophagus
P0468 - Efficacy and Safety of Argon Plasma Coagulation and Radiofrequency Ablation for the Management of Gastric Inlet Patches: A Systematic Review and Meta-Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- RW
Reid Wasserman, DO
Carilion Clinic Virginia Tech
Roanoke, VA
Presenting Author(s)
Reid Wasserman, DO1, Vishali Moond, MD2, Paul Yeaton, MD1, Patrick Okolo, MD1, Vivek Kesar, MD3, Babu Mohan, MD4, Varun Kesar, MD3
1Carilion Clinic Virginia Tech, Roanoke, VA; 2Saint Peter's University Hospital, New Brunswick, NJ; 3Carilion Clinic, Roanoke, VA; 4Orlando Gastroenterology PA, Orlando, FL
Introduction: Gastric inlet Patches (GIP) are isolated areas of heterotopic gastric mucosa that are implanted in the esophageal mucosa. They have a prevalence of up to 10% in the population and are largely found incidentally on upper endoscopy; however, GIPs can be symptomatic and can present as globus sensation, sore throat, dysphagia, and hoarseness. Patients are often trialed on proton pump inhibitor therapy (PPI) as an initial therapeutic treatment with limited clinical efficacy. Argon plasma coagulation (APC) and radiofrequency ablation (RFA) are two methods of ablating heterotopic gastric tissue that have been studied for symptom relief and definitive treatment for GIPs.
Methods: We conducted a literature review using Pubmed, SCOPUS, and Cochrane Library from inception to May 2024 to identify studies that evaluated the efficacy and safety of APC/RFA for the management of GIPs. The primary outcomes of interest were clinical success (defined by overall symptomatic improvement in globus sensation, sore throat, dysphagia, hoarseness, cough, or heart burn) and major adverse events. Random-effects model was used to calculate pooled rates and I2 values were used to assess heterogeneity.
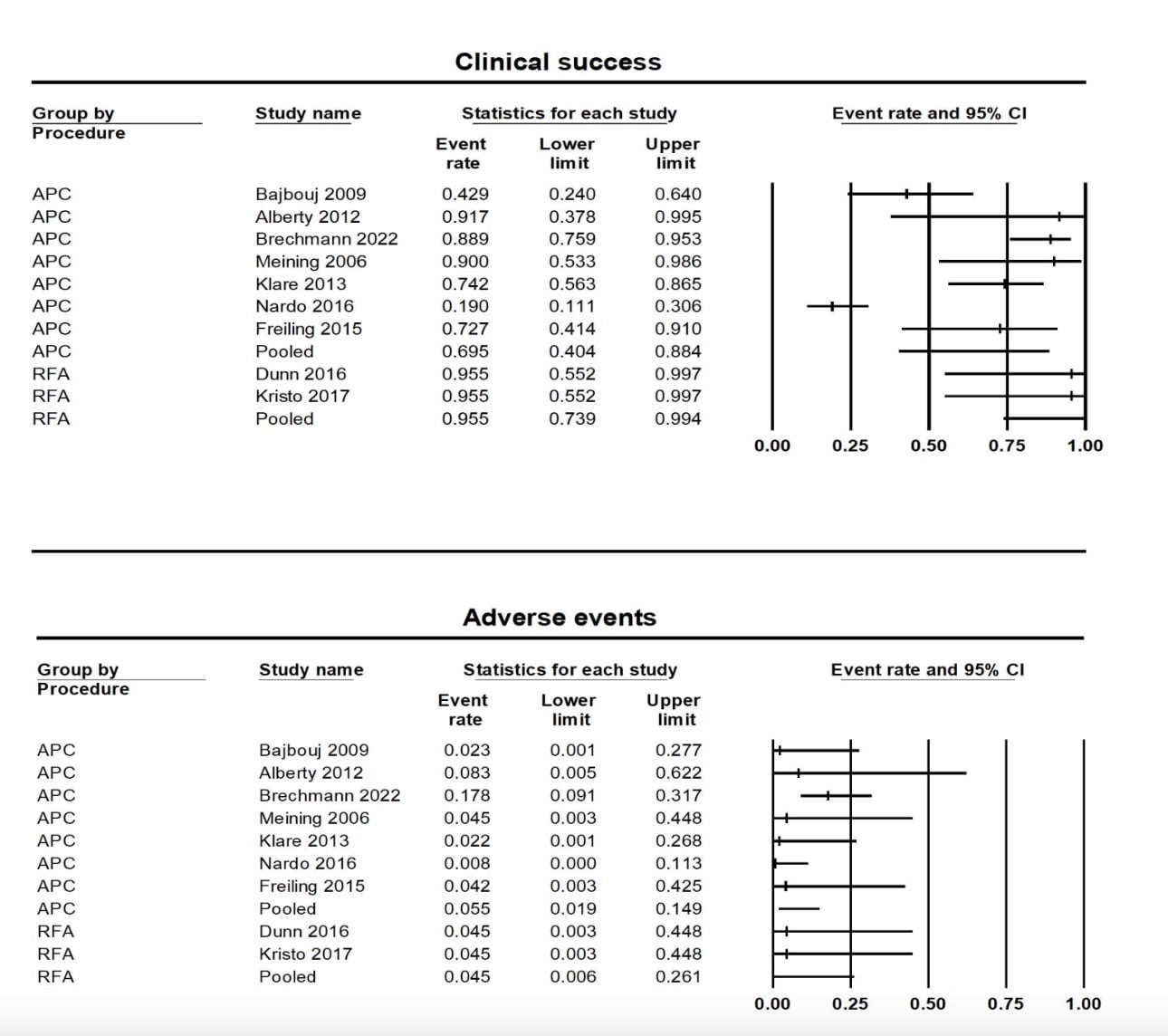
Results: Our meta-analysis included nine studies with 131 symptomatic patients who underwent APC/RFA for management of GIPs. Two studies included 20 patients who underwent RFA ablation, and seven studies included 111 patients who underwent APC ablation. Of the studies, one was a randomized controlled trial, and 8 were observational studies. The pooled rate for clinical success for APC was 69.5% (95% confidence interval [CI] 40.4% - 88.4%; I2= 89%) and 95.5% [73.9% - 99.4%; I2= 0%] for RFA. The adverse event rate for APC was 5.5% [1.9% - 14.9%; I2= 37%] and 4.5% [0.6% - 26.1%; I2= 0%] for RFA. Results are summarized in Figure 1.
Discussion: Based on this meta-analysis, APC and RFA are effective and safe treatments for gastric inlet patches, which have shown to reduce overall symptoms with a low adverse event rate. The subgroup analysis showed that RFA appears to be more effective than APC; however more studies with RFA should be conducted for confirmation.
Disclosures:
Reid Wasserman, DO1, Vishali Moond, MD2, Paul Yeaton, MD1, Patrick Okolo, MD1, Vivek Kesar, MD3, Babu Mohan, MD4, Varun Kesar, MD3. P0468 - Efficacy and Safety of Argon Plasma Coagulation and Radiofrequency Ablation for the Management of Gastric Inlet Patches: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Carilion Clinic Virginia Tech, Roanoke, VA; 2Saint Peter's University Hospital, New Brunswick, NJ; 3Carilion Clinic, Roanoke, VA; 4Orlando Gastroenterology PA, Orlando, FL
Introduction: Gastric inlet Patches (GIP) are isolated areas of heterotopic gastric mucosa that are implanted in the esophageal mucosa. They have a prevalence of up to 10% in the population and are largely found incidentally on upper endoscopy; however, GIPs can be symptomatic and can present as globus sensation, sore throat, dysphagia, and hoarseness. Patients are often trialed on proton pump inhibitor therapy (PPI) as an initial therapeutic treatment with limited clinical efficacy. Argon plasma coagulation (APC) and radiofrequency ablation (RFA) are two methods of ablating heterotopic gastric tissue that have been studied for symptom relief and definitive treatment for GIPs.
Methods: We conducted a literature review using Pubmed, SCOPUS, and Cochrane Library from inception to May 2024 to identify studies that evaluated the efficacy and safety of APC/RFA for the management of GIPs. The primary outcomes of interest were clinical success (defined by overall symptomatic improvement in globus sensation, sore throat, dysphagia, hoarseness, cough, or heart burn) and major adverse events. Random-effects model was used to calculate pooled rates and I2 values were used to assess heterogeneity.
Results: Our meta-analysis included nine studies with 131 symptomatic patients who underwent APC/RFA for management of GIPs. Two studies included 20 patients who underwent RFA ablation, and seven studies included 111 patients who underwent APC ablation. Of the studies, one was a randomized controlled trial, and 8 were observational studies. The pooled rate for clinical success for APC was 69.5% (95% confidence interval [CI] 40.4% - 88.4%; I2= 89%) and 95.5% [73.9% - 99.4%; I2= 0%] for RFA. The adverse event rate for APC was 5.5% [1.9% - 14.9%; I2= 37%] and 4.5% [0.6% - 26.1%; I2= 0%] for RFA. Results are summarized in Figure 1.
Discussion: Based on this meta-analysis, APC and RFA are effective and safe treatments for gastric inlet patches, which have shown to reduce overall symptoms with a low adverse event rate. The subgroup analysis showed that RFA appears to be more effective than APC; however more studies with RFA should be conducted for confirmation.
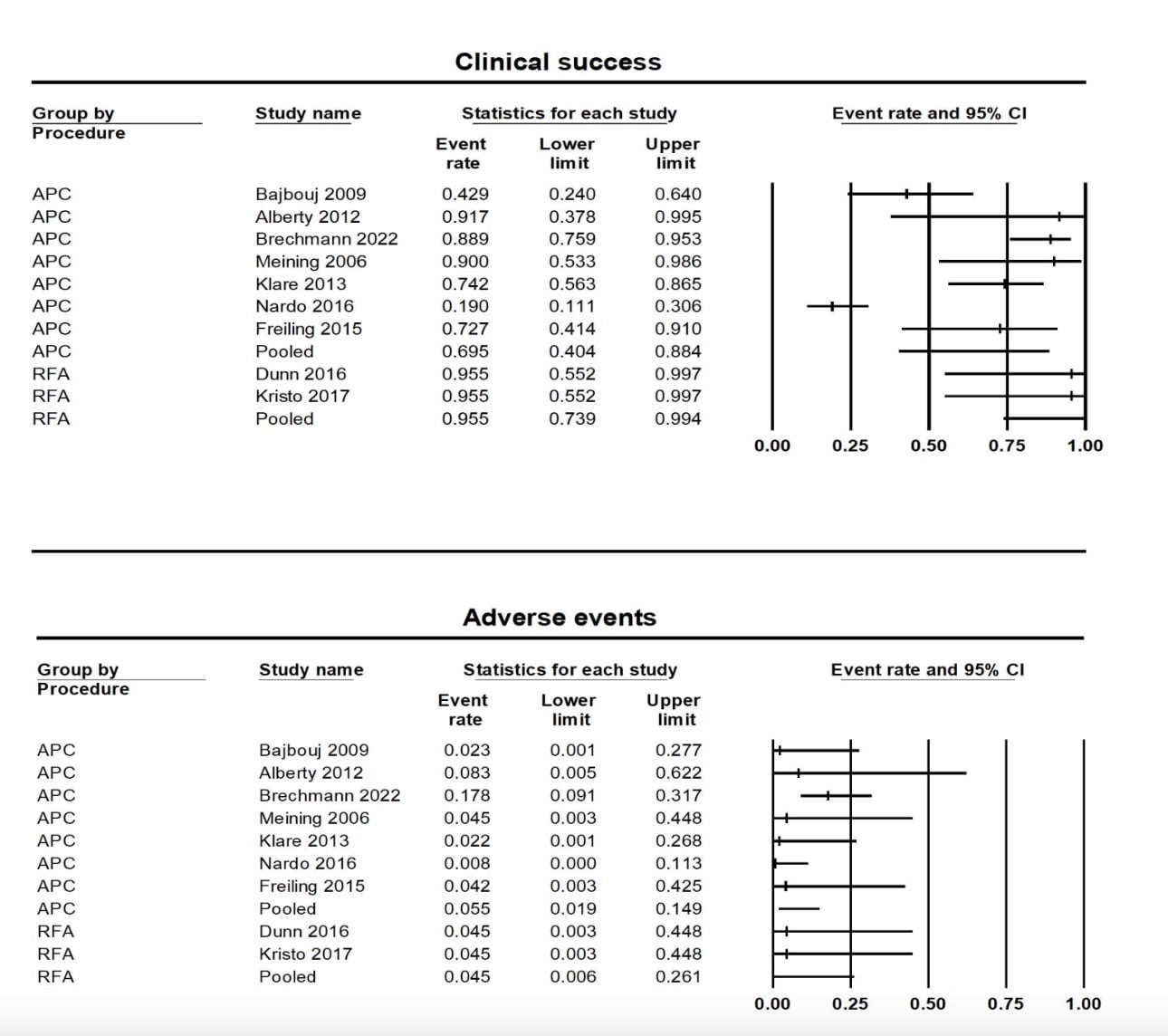
Figure: Figure 1. Clinical success and adverse event rate of APC/RFA for management of gastric inlet patches
Disclosures:
Reid Wasserman indicated no relevant financial relationships.
Vishali Moond indicated no relevant financial relationships.
Paul Yeaton indicated no relevant financial relationships.
Patrick Okolo indicated no relevant financial relationships.
Vivek Kesar indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Varun Kesar indicated no relevant financial relationships.
Reid Wasserman, DO1, Vishali Moond, MD2, Paul Yeaton, MD1, Patrick Okolo, MD1, Vivek Kesar, MD3, Babu Mohan, MD4, Varun Kesar, MD3. P0468 - Efficacy and Safety of Argon Plasma Coagulation and Radiofrequency Ablation for the Management of Gastric Inlet Patches: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
