Sunday Poster Session
Category: Esophagus
P0470 - Assessing the Impact of Age on Barrett’s Esophagus in Patient With Gastrectomy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Het Patel, DO
St. Luke's University Hospital
Bethlehem, PA
Presenting Author(s)
Het Patel, DO1, Nisha Sanghani, DO2, Ibrahim Ragab, DO3, Pooja D.. Patel, DO4, Hammad Liaquat, MD2
1St. Luke's University Hospital, Bethlehem, PA; 2St. Luke's University Health Network, Bethlehem, PA; 3Saint Luke's University Hospital, Bethlehem, PA; 4St. Luke’s University Health Network, Bethlehem, PA
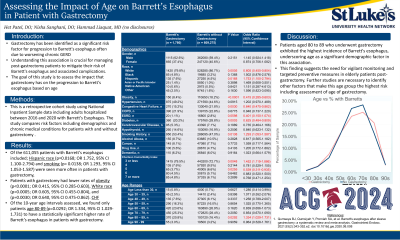
Introduction: Gastrectomy has been identified as a significant risk factor for progression to Barrett's esophagus often due to worsening chronic gastroesophageal reflux disease (GERD). Understanding this association is crucial for managing post-gastrectomy patients to mitigate their risk of developing Barrett's esophagus and associated complications. The goal of this study is to assess the impact that gastrectomy has on the progression to Barrett’s esophagus based on age.
Methods: This is a retrospective cohort study using National Inpatient Sample data including all adult patients hospitalized between 2016 and 2020 who were found to have Barrett’s esophagus. The study compares risk factors including demographics and chronic medical conditions for patients with and without gastrectomy. Statistical analyses were all performed using STATA software.
Results: Of the 611,055 patients with Barrett’s esophagus included in our study, gender, Black race, Asian/Pacific Islander, Native American, other race, hypertension, COPD, ESRD, cerebrovascular disease, hypothyroidism, alcohol abuse, cancer, other drug use, and dementia did not have a statistically significant effect (p >0.05) on our two groups. Hispanic race (p=0.0168; OR 1.752, 95% CI 1.100-2.794) and smoking (p= 0.0138; OR 1.293, 95% CI 1.053-1.587) were seen more often in patients with gastrectomy, and patients with gastrectomy had lower rates of obesity (p< 0.0001; OR 0.415, 95% CI 0.285-0.603), smoking history (p=0.0138; OR 1.293 95% CI 1.053-1.587), White race (p=0.0005; OR 0.605, 95% CI 0.455-0.804), and congestive heart failure (p=0.0030; OR 0.640, 95% CI 0.475-0.862). Of the 10-year age intervals assessed, we found only patients age 80-89 (p=0.0292; OR 1.334, 95% CI 1.029-1.731) to have a statistically significant higher rate of Barrett’s esophagus in patients with gastrectomy (Table 1).
Discussion: Patients aged 80 to 89 who underwent gastrectomy exhibited the highest incidence of Barrett's esophagus, underscoring age as a significant demographic factor in this association. This finding suggests the need for vigilant monitoring and targeted preventive measures in elderly patients post-gastrectomy. Further studies are necessary to identify other factors that make this age group the highest risk.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Het Patel, DO1, Nisha Sanghani, DO2, Ibrahim Ragab, DO3, Pooja D.. Patel, DO4, Hammad Liaquat, MD2. P0470 - Assessing the Impact of Age on Barrett’s Esophagus in Patient With Gastrectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Luke's University Hospital, Bethlehem, PA; 2St. Luke's University Health Network, Bethlehem, PA; 3Saint Luke's University Hospital, Bethlehem, PA; 4St. Luke’s University Health Network, Bethlehem, PA
Introduction: Gastrectomy has been identified as a significant risk factor for progression to Barrett's esophagus often due to worsening chronic gastroesophageal reflux disease (GERD). Understanding this association is crucial for managing post-gastrectomy patients to mitigate their risk of developing Barrett's esophagus and associated complications. The goal of this study is to assess the impact that gastrectomy has on the progression to Barrett’s esophagus based on age.
Methods: This is a retrospective cohort study using National Inpatient Sample data including all adult patients hospitalized between 2016 and 2020 who were found to have Barrett’s esophagus. The study compares risk factors including demographics and chronic medical conditions for patients with and without gastrectomy. Statistical analyses were all performed using STATA software.
Results: Of the 611,055 patients with Barrett’s esophagus included in our study, gender, Black race, Asian/Pacific Islander, Native American, other race, hypertension, COPD, ESRD, cerebrovascular disease, hypothyroidism, alcohol abuse, cancer, other drug use, and dementia did not have a statistically significant effect (p >0.05) on our two groups. Hispanic race (p=0.0168; OR 1.752, 95% CI 1.100-2.794) and smoking (p= 0.0138; OR 1.293, 95% CI 1.053-1.587) were seen more often in patients with gastrectomy, and patients with gastrectomy had lower rates of obesity (p< 0.0001; OR 0.415, 95% CI 0.285-0.603), smoking history (p=0.0138; OR 1.293 95% CI 1.053-1.587), White race (p=0.0005; OR 0.605, 95% CI 0.455-0.804), and congestive heart failure (p=0.0030; OR 0.640, 95% CI 0.475-0.862). Of the 10-year age intervals assessed, we found only patients age 80-89 (p=0.0292; OR 1.334, 95% CI 1.029-1.731) to have a statistically significant higher rate of Barrett’s esophagus in patients with gastrectomy (Table 1).
Discussion: Patients aged 80 to 89 who underwent gastrectomy exhibited the highest incidence of Barrett's esophagus, underscoring age as a significant demographic factor in this association. This finding suggests the need for vigilant monitoring and targeted preventive measures in elderly patients post-gastrectomy. Further studies are necessary to identify other factors that make this age group the highest risk.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Het Patel indicated no relevant financial relationships.
Nisha Sanghani indicated no relevant financial relationships.
Ibrahim Ragab indicated no relevant financial relationships.
Pooja Patel indicated no relevant financial relationships.
Hammad Liaquat indicated no relevant financial relationships.
Het Patel, DO1, Nisha Sanghani, DO2, Ibrahim Ragab, DO3, Pooja D.. Patel, DO4, Hammad Liaquat, MD2. P0470 - Assessing the Impact of Age on Barrett’s Esophagus in Patient With Gastrectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
