Sunday Poster Session
Category: Esophagus
P0471 - Patriot Clinic Proton-Pump Inhibitor Review and Therapy De-Escalation (PCP-PIRATE) at the Orlando VA Healthcare System
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Sonia Alicea, MD
Orlando VA Medical Center and UCF/HCA Greater Orlando
Kissimmee, FL
Presenting Author(s)
Sonia Alicea, MD1, Emmanuel Magsino, MD, MS1, Sriya Reddy, MD1, Alfredo Palomino Abella, MD1, Faris Abby Alamin, MD1, Raj Shah, MD1, Ashwini Komarla, MD2, David Simmons, MD2, Amar Mandalia, MD, FACG2
1Orlando VA Medical Center and UCF/HCA Greater Orlando, Kissimmee, FL; 2Orlando VA Medical Center and UCF/HCA Greater Orlando, Orlando, FL
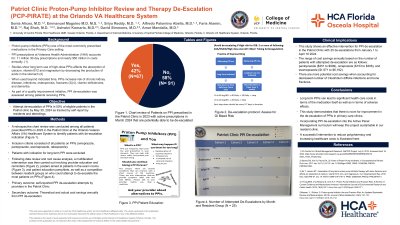
Introduction: Proton pump inhibitors (PPIs) are one of the most commonly prescribed medications. PPI prescriptions at Veterans Health Administration accounts for over 11 million 30-day prescriptions and nearly $50 million in medication costs annually. PPIs long term use affects absorption of calcium, vitamin B12 and magnesium by decreasing stomach acid production. When used beyond the indicated time, PPIs increase the risk of chronic kidney disease, infections, osteoporosis, fractures, vitamin deficiencies, and dementia, contributing to polypharmacy and increasing healthcare costs. The objective of this project was to attempt de-escalation of PPIs in 50% of eligible patients in the resident run Patriot Clinic by May 30, 2024 as tracked by self report by residents and attendings.
Methods: A retrospective chart review was conducted among all patients prescribed PPIs in 2023 in the Patriot Clinic in the Orlando VA Healthcare System to identify the baseline number of patients who can be de-escalated. Inclusion criteria consisted of all patients on PPIs. Patients with indication for long term PPI were excluded. Following root cause analysis, the interventions involved provider education and reminders, posters directed at patients in the exam rooms and patient education pamphlets, as well as a competition between resident groups to attempt de-escalation of PPIs for their patients. The primary outcome was the number of self-reported PPI de-escalation attempts by clinic providers. Secondary outcomes included theoretical and actual cost savings annually based on the cost of each medication through the VA per the number of potential and attempted PPI de-escalations.
Results: Out of 158 patients chart reviewed, 67 patients (42%) had potential for PPI de-escalation. Twenty-five patients attempted de-escalation by May 2024. The range of cost savings annually based on the number of patients with attempted de-escalation are as follows: pantoprazole ($351 to $909), omeprazole ($153 to $306), and esomeprazole ($1,971 to $6,192). There are more potential cost savings when accounting for avoidance of complications.
Discussion: Long term PPIs can lead to significant health care costs in terms of the medication itself and adverse effects. This study shows an effective intervention for PPI de-escalation in our resident clinic with 25 de-escalations from January to May 2024; with a notable theoretical and actual cost savings. As demonstrated, there is room for improvement in the de-escalation of PPIs in primary care clinics.
Disclosures:
Sonia Alicea, MD1, Emmanuel Magsino, MD, MS1, Sriya Reddy, MD1, Alfredo Palomino Abella, MD1, Faris Abby Alamin, MD1, Raj Shah, MD1, Ashwini Komarla, MD2, David Simmons, MD2, Amar Mandalia, MD, FACG2. P0471 - Patriot Clinic Proton-Pump Inhibitor Review and Therapy De-Escalation (PCP-PIRATE) at the Orlando VA Healthcare System, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Orlando VA Medical Center and UCF/HCA Greater Orlando, Kissimmee, FL; 2Orlando VA Medical Center and UCF/HCA Greater Orlando, Orlando, FL
Introduction: Proton pump inhibitors (PPIs) are one of the most commonly prescribed medications. PPI prescriptions at Veterans Health Administration accounts for over 11 million 30-day prescriptions and nearly $50 million in medication costs annually. PPIs long term use affects absorption of calcium, vitamin B12 and magnesium by decreasing stomach acid production. When used beyond the indicated time, PPIs increase the risk of chronic kidney disease, infections, osteoporosis, fractures, vitamin deficiencies, and dementia, contributing to polypharmacy and increasing healthcare costs. The objective of this project was to attempt de-escalation of PPIs in 50% of eligible patients in the resident run Patriot Clinic by May 30, 2024 as tracked by self report by residents and attendings.
Methods: A retrospective chart review was conducted among all patients prescribed PPIs in 2023 in the Patriot Clinic in the Orlando VA Healthcare System to identify the baseline number of patients who can be de-escalated. Inclusion criteria consisted of all patients on PPIs. Patients with indication for long term PPI were excluded. Following root cause analysis, the interventions involved provider education and reminders, posters directed at patients in the exam rooms and patient education pamphlets, as well as a competition between resident groups to attempt de-escalation of PPIs for their patients. The primary outcome was the number of self-reported PPI de-escalation attempts by clinic providers. Secondary outcomes included theoretical and actual cost savings annually based on the cost of each medication through the VA per the number of potential and attempted PPI de-escalations.
Results: Out of 158 patients chart reviewed, 67 patients (42%) had potential for PPI de-escalation. Twenty-five patients attempted de-escalation by May 2024. The range of cost savings annually based on the number of patients with attempted de-escalation are as follows: pantoprazole ($351 to $909), omeprazole ($153 to $306), and esomeprazole ($1,971 to $6,192). There are more potential cost savings when accounting for avoidance of complications.
Discussion: Long term PPIs can lead to significant health care costs in terms of the medication itself and adverse effects. This study shows an effective intervention for PPI de-escalation in our resident clinic with 25 de-escalations from January to May 2024; with a notable theoretical and actual cost savings. As demonstrated, there is room for improvement in the de-escalation of PPIs in primary care clinics.
Disclosures:
Sonia Alicea indicated no relevant financial relationships.
Emmanuel Magsino indicated no relevant financial relationships.
Sriya Reddy indicated no relevant financial relationships.
Alfredo Palomino Abella indicated no relevant financial relationships.
Faris Abby Alamin indicated no relevant financial relationships.
Raj Shah indicated no relevant financial relationships.
Ashwini Komarla indicated no relevant financial relationships.
David Simmons indicated no relevant financial relationships.
Amar Mandalia indicated no relevant financial relationships.
Sonia Alicea, MD1, Emmanuel Magsino, MD, MS1, Sriya Reddy, MD1, Alfredo Palomino Abella, MD1, Faris Abby Alamin, MD1, Raj Shah, MD1, Ashwini Komarla, MD2, David Simmons, MD2, Amar Mandalia, MD, FACG2. P0471 - Patriot Clinic Proton-Pump Inhibitor Review and Therapy De-Escalation (PCP-PIRATE) at the Orlando VA Healthcare System, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

