Sunday Poster Session
Category: Esophagus
P0477 - Gastroesophageal Reflux Disease After Heller Myotomy: Can Concomitant Fundoplication Aid in Prevention? A Comparative Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Abdul-Rahman F. Diab, MD
University of South Florida Morsani College of Medicine and University of Central Florida, HCA Healthcare GME
Ocala, FL
Presenting Author(s)
Abdul-Rahman F. Diab, MD1, Joseph A. Sujka, MD2, Kathleen Mattingly, DO3, Angelica McCaskey, DO3, Abdullah Elnaji, DO3, Salvatore Docimo, DO2, Christopher G. DuCoin, MD2
1University of South Florida Morsani College of Medicine and University of Central Florida, HCA Healthcare GME, Ocala, FL; 2University of South Florida Morsani College of Medicine, Tampa, FL; 3University of Central Florida, HCA Healthcare GME, Ocala, FL
Introduction: Gastroesophageal reflux disease (GERD) is a common complication following Heller myotomy. Consequently, many surgeons perform concurrent fundoplication to mitigate the incidence of GERD. The most utilized technique in conjunction with Heller myotomy is the Dor/anterior hemifundoplication (180 degrees), with Toupet (270 degrees) and Nissen (360 degrees) fundoplications being less commonly used. There is no clear evidence in the literature to support the efficacy of adding fundoplication to Heller myotomy for reducing the incidence of postoperative GERD. Therefore, we aimed to compare Heller myotomy (HM) alone versus Heller myotomy with fundoplication (HMF) through a pairwise meta-analysis of comparative studies.
Methods: We conducted a systematic literature review following PRISMA guidelines to identify articles that directly compare HM and HMF in patients with achalasia. We utilized the random effects model and calculated odds ratios for dichotomous data, and mean differences for continuous data, as metrics for effect size. Subgroup analysis was performed according to study methodology (randomized and non-randomized) and fundoplication technique (Dor, Toupet, and Nissen).
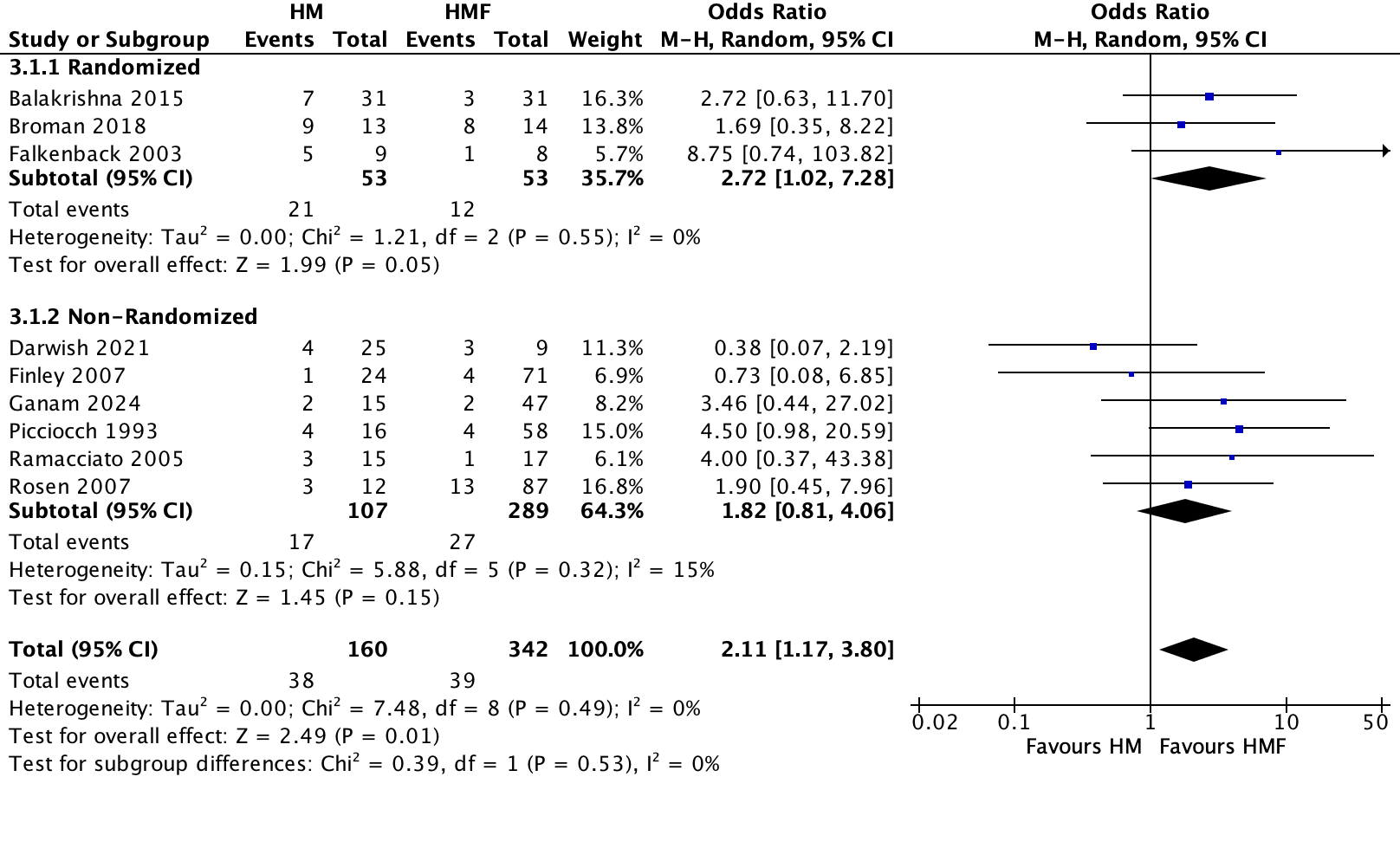
Results: Nine studies were included in the analysis: three were randomized, and six were non-randomized. The incidence of GERD was reported in all nine studies, with 160 cases in the HM group and 342 cases in the HMF group. A statistically significant increase in the incidence of GERD was observed with HM compared to HMF (OR 2.11, 95% CI 1.17–3.80, p = 0.01). The increased incidence was consistent with no heterogeneity among the studies (I² = 0%, p = 0.49). The number needed to treat with HM to result in one harmful event (a case of GERD) was 10 (95% CI 5–59). Subgroup analysis according to study methodology and fundoplication technique did not reveal significant differences. Interestingly, when subgrouping according to methodology, randomized controlled trials (RCTs) alone showed a statistically significant increase in the incidence of GERD with HM compared to HMF, supporting the efficacy of fundoplication based on RCT-level evidence.
Discussion: This study suggests that adding fundoplication at the time of Heller myotomy can reduce the incidence of GERD. However, many of the studies included are historic, and new data are needed, especially with the advent of new surgical techniques.
Disclosures:
Abdul-Rahman F. Diab, MD1, Joseph A. Sujka, MD2, Kathleen Mattingly, DO3, Angelica McCaskey, DO3, Abdullah Elnaji, DO3, Salvatore Docimo, DO2, Christopher G. DuCoin, MD2. P0477 - Gastroesophageal Reflux Disease After Heller Myotomy: Can Concomitant Fundoplication Aid in Prevention? A Comparative Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of South Florida Morsani College of Medicine and University of Central Florida, HCA Healthcare GME, Ocala, FL; 2University of South Florida Morsani College of Medicine, Tampa, FL; 3University of Central Florida, HCA Healthcare GME, Ocala, FL
Introduction: Gastroesophageal reflux disease (GERD) is a common complication following Heller myotomy. Consequently, many surgeons perform concurrent fundoplication to mitigate the incidence of GERD. The most utilized technique in conjunction with Heller myotomy is the Dor/anterior hemifundoplication (180 degrees), with Toupet (270 degrees) and Nissen (360 degrees) fundoplications being less commonly used. There is no clear evidence in the literature to support the efficacy of adding fundoplication to Heller myotomy for reducing the incidence of postoperative GERD. Therefore, we aimed to compare Heller myotomy (HM) alone versus Heller myotomy with fundoplication (HMF) through a pairwise meta-analysis of comparative studies.
Methods: We conducted a systematic literature review following PRISMA guidelines to identify articles that directly compare HM and HMF in patients with achalasia. We utilized the random effects model and calculated odds ratios for dichotomous data, and mean differences for continuous data, as metrics for effect size. Subgroup analysis was performed according to study methodology (randomized and non-randomized) and fundoplication technique (Dor, Toupet, and Nissen).
Results: Nine studies were included in the analysis: three were randomized, and six were non-randomized. The incidence of GERD was reported in all nine studies, with 160 cases in the HM group and 342 cases in the HMF group. A statistically significant increase in the incidence of GERD was observed with HM compared to HMF (OR 2.11, 95% CI 1.17–3.80, p = 0.01). The increased incidence was consistent with no heterogeneity among the studies (I² = 0%, p = 0.49). The number needed to treat with HM to result in one harmful event (a case of GERD) was 10 (95% CI 5–59). Subgroup analysis according to study methodology and fundoplication technique did not reveal significant differences. Interestingly, when subgrouping according to methodology, randomized controlled trials (RCTs) alone showed a statistically significant increase in the incidence of GERD with HM compared to HMF, supporting the efficacy of fundoplication based on RCT-level evidence.
Discussion: This study suggests that adding fundoplication at the time of Heller myotomy can reduce the incidence of GERD. However, many of the studies included are historic, and new data are needed, especially with the advent of new surgical techniques.
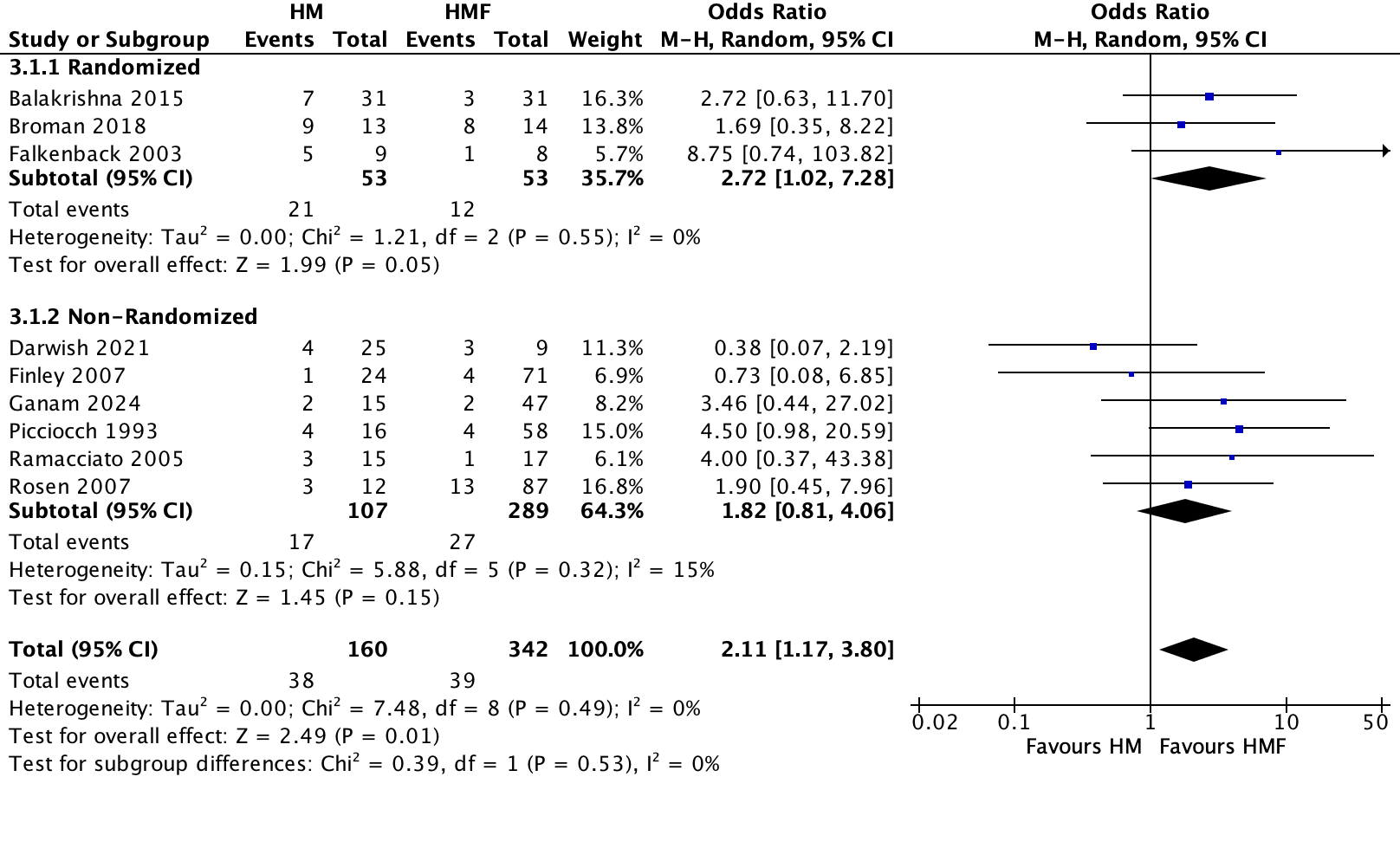
Figure: Forest plot comparing Heller myotomy (HM) and Heller myotomy with fundoplication (HMF) in postoperative gastroesophageal reflux disease (GERD).
Disclosures:
Abdul-Rahman Diab indicated no relevant financial relationships.
Joseph Sujka indicated no relevant financial relationships.
Kathleen Mattingly indicated no relevant financial relationships.
Angelica McCaskey indicated no relevant financial relationships.
Abdullah Elnaji indicated no relevant financial relationships.
Salvatore Docimo indicated no relevant financial relationships.
Christopher DuCoin indicated no relevant financial relationships.
Abdul-Rahman F. Diab, MD1, Joseph A. Sujka, MD2, Kathleen Mattingly, DO3, Angelica McCaskey, DO3, Abdullah Elnaji, DO3, Salvatore Docimo, DO2, Christopher G. DuCoin, MD2. P0477 - Gastroesophageal Reflux Disease After Heller Myotomy: Can Concomitant Fundoplication Aid in Prevention? A Comparative Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
