Sunday Poster Session
Category: Colon
P0380 - A Case of Undifferentiated Colitis in a Patient With Liver Transplant and Crohn’s Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Tanner Thornsberry, MD
University of Cincinnati Medical Center
Cincinnati, OH
Presenting Author(s)
Tanner Thornsberry, MD1, Jacob A. Ciricillo, MD2, Benjamin Clement, MD1, Kara DeFelice, MD3
1University of Cincinnati Medical Center, Cincinnati, OH; 2University of Cincinnati, Cincinnati, OH; 3University of Cincinnati College of Medicine, Cincinnati, OH
Introduction: The majority of patients with primary sclerosing cholangitis (PSC) have coexisting inflammatory bowel disease (IBD) and a significant portion eventually require liver transplantation. It has been established that the postoperative transplant period for this patient population carries significant risk of IBD relapse. In such patients who present with gastrointestinal distress, the differential is broad and includes opportunistic infectious etiologies, graft-versus-host disease, drug-toxicity, and IBD.
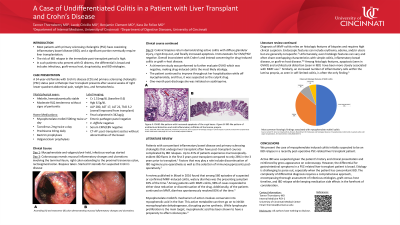
Case Description/Methods: A 34 year old woman with Crohn’s Disease (CD) and primary sclerosing cholangitis (PSC) status post orthotopic liver transplant was admitted to the hospital after several weeks of right lower quadrant abdominal pain, decreased appetite, weight loss, and hematochezia. The patient’s medications included mycophenolate mofetil, tacrolimus, and prednisone. Her mycophenolate was held.
The patient was afebrile with normal vital signs. Physical exam was notable for right lower quadrant tenderness. Initial laboratory workup revealed liver chemistries that were elevated but overall improving from transplant. Imaging did not demonstrate any abnormalities involving the bowel. Fecal calprotectin was found to be elevated. Colonoscopy revealed mucosal inflammatory changes and ulcerations involving the terminal ileum and large portions of the colon. The patient was subsequently started on IV steroids for suspected active CD. Biopsy results later revealed active colitis with diffuse glandular injury, crypt drop-out, and focally increased apoptosis. Immunostaining and GVHD testing were unremarkable. From the biopsies, it was determined that drug-induced colitis from mycophenolate was the most likely etiology. The patient’s symptoms continued to improve off of mycophenolate.
Discussion: Patients with IBD that undergo transplantation are known to be at high risk for IBD relapse due to perioperative changes to immunosuppression. Active IBD was suspected given the patient’s history and clinical presentation, and reinforced by gross appearance on colonoscopy. However, the differential for gastrointestinal symptoms in a PSC-related liver transplant patient is broad. Etiology is challenging to parse out, especially when the patient has concomitant IBD. The complexity of differential diagnosis requires a comprehensive approach, encompassing thorough assessment of infectious etiologies, graft-versus-host timeline, and IBD relapse while keeping medication side effects in the forefront of consideration.
Disclosures:
Tanner Thornsberry, MD1, Jacob A. Ciricillo, MD2, Benjamin Clement, MD1, Kara DeFelice, MD3. P0380 - A Case of Undifferentiated Colitis in a Patient With Liver Transplant and Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Cincinnati Medical Center, Cincinnati, OH; 2University of Cincinnati, Cincinnati, OH; 3University of Cincinnati College of Medicine, Cincinnati, OH
Introduction: The majority of patients with primary sclerosing cholangitis (PSC) have coexisting inflammatory bowel disease (IBD) and a significant portion eventually require liver transplantation. It has been established that the postoperative transplant period for this patient population carries significant risk of IBD relapse. In such patients who present with gastrointestinal distress, the differential is broad and includes opportunistic infectious etiologies, graft-versus-host disease, drug-toxicity, and IBD.
Case Description/Methods: A 34 year old woman with Crohn’s Disease (CD) and primary sclerosing cholangitis (PSC) status post orthotopic liver transplant was admitted to the hospital after several weeks of right lower quadrant abdominal pain, decreased appetite, weight loss, and hematochezia. The patient’s medications included mycophenolate mofetil, tacrolimus, and prednisone. Her mycophenolate was held.
The patient was afebrile with normal vital signs. Physical exam was notable for right lower quadrant tenderness. Initial laboratory workup revealed liver chemistries that were elevated but overall improving from transplant. Imaging did not demonstrate any abnormalities involving the bowel. Fecal calprotectin was found to be elevated. Colonoscopy revealed mucosal inflammatory changes and ulcerations involving the terminal ileum and large portions of the colon. The patient was subsequently started on IV steroids for suspected active CD. Biopsy results later revealed active colitis with diffuse glandular injury, crypt drop-out, and focally increased apoptosis. Immunostaining and GVHD testing were unremarkable. From the biopsies, it was determined that drug-induced colitis from mycophenolate was the most likely etiology. The patient’s symptoms continued to improve off of mycophenolate.
Discussion: Patients with IBD that undergo transplantation are known to be at high risk for IBD relapse due to perioperative changes to immunosuppression. Active IBD was suspected given the patient’s history and clinical presentation, and reinforced by gross appearance on colonoscopy. However, the differential for gastrointestinal symptoms in a PSC-related liver transplant patient is broad. Etiology is challenging to parse out, especially when the patient has concomitant IBD. The complexity of differential diagnosis requires a comprehensive approach, encompassing thorough assessment of infectious etiologies, graft-versus-host timeline, and IBD relapse while keeping medication side effects in the forefront of consideration.
Disclosures:
Tanner Thornsberry indicated no relevant financial relationships.
Jacob Ciricillo indicated no relevant financial relationships.
Benjamin Clement indicated no relevant financial relationships.
Kara DeFelice: Abbvie – Advisory Committee/Board Member, Speakers Bureau. BMS – Advisory Committee/Board Member, Speakers Bureau. Janssen – Honorary Speaker.
Tanner Thornsberry, MD1, Jacob A. Ciricillo, MD2, Benjamin Clement, MD1, Kara DeFelice, MD3. P0380 - A Case of Undifferentiated Colitis in a Patient With Liver Transplant and Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
