Sunday Poster Session
Category: Colon
P0385 - An Outbreak of Shigella Dysentery at an Urban Tertiary Care Hospital
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Lindsay Matthews, MD
Temple University
Philadelphia, PA
Presenting Author(s)
Lindsay Matthews, MD1, Christa Smaltz, MD1, Holly Greenwald, MD2
1Temple University, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Introduction: In the United States, Shigella is associated with poverty and crowded living conditions owing to its high virulence. The two most common isolates are Shigella soneii and Shigella flexneri, the latter of which is less common but causes a more severe course.
Shigella is spread through the fecal-oral route, via sexual contact and contaminated food/water. The incubation period is 1-3 days and symptoms usually self-resolve within 7 days. The main affected area is the rectosigmoid colon. Bacteremia is rare and is more common in adults >65 years or with comorbid diabetes. Symptoms generally start with watery diarrhea, later with bloody diarrhea and tenesmus. There is emergence of drug-resistant strains.
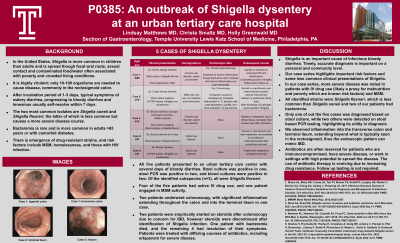
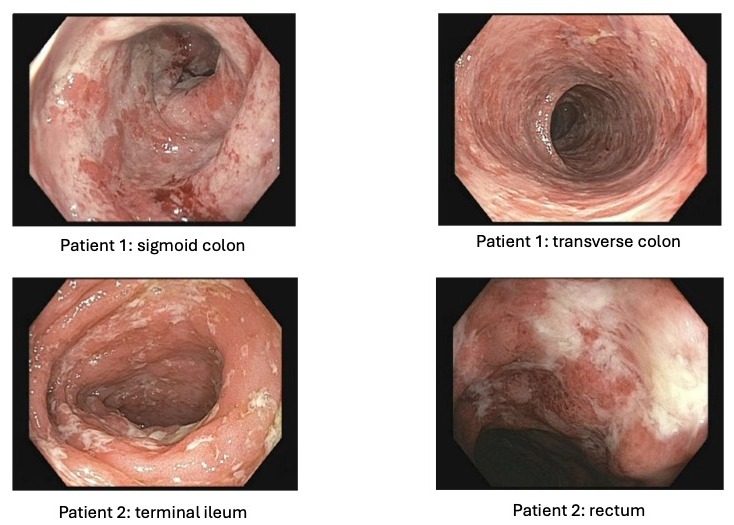
Case Description/Methods: Here we present 5 cases of Shigella dysentery at an urban tertiary care center. All five patients presented with several days of bloody diarrhea. Stool culture was positive in one, PCR was positive in two, and blood cultures were positive in two. Of the identified subspecies (n=3), all were Shigella flexneri. Four of the five patients had active IV drug use, and one patient engaged in MSM. Two patients underwent colonoscopy, with significant inflammation extending throughout the colon, and into the terminal ileum in one case.
Two patients were empirically started on steroids after colonoscopy due to concern for IBD, however steroids were discontinued after identification of Shigella infection. One patient with bacteremia died, and the remaining 4 had resolution of their symptoms. Patients were treated with differing courses of antibiotics, including ertapenem for severe disease.
Discussion: Shigella is an important cause of infectious bloody diarrhea, and timely diagnosis is important on a personal and community level. The pattern of inflammation can mimic IBD, and our case series highlights more severe disease in patients with IV drug use (likely a proxy for malnutrition and poverty) and MSM. All identified strains were Shigella flexneri, which is less common than Shigella soneii although typically causes a more severe course; two of our patients had bacteremia. Only one of out the five cases was diagnosed based on stool culture. We observed inflammation into the ascending colon and TI, extending beyond what is typically seen in the rectosigmoid. Antibiotics are often reserved for patients who are immunocompromised or have severe disease, although there increasing drug resistance. Follow up testing is not required.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Lindsay Matthews, MD1, Christa Smaltz, MD1, Holly Greenwald, MD2. P0385 - An Outbreak of <i>Shigella</i> Dysentery at an Urban Tertiary Care Hospital, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Temple University, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Introduction: In the United States, Shigella is associated with poverty and crowded living conditions owing to its high virulence. The two most common isolates are Shigella soneii and Shigella flexneri, the latter of which is less common but causes a more severe course.
Shigella is spread through the fecal-oral route, via sexual contact and contaminated food/water. The incubation period is 1-3 days and symptoms usually self-resolve within 7 days. The main affected area is the rectosigmoid colon. Bacteremia is rare and is more common in adults >65 years or with comorbid diabetes. Symptoms generally start with watery diarrhea, later with bloody diarrhea and tenesmus. There is emergence of drug-resistant strains.
Case Description/Methods: Here we present 5 cases of Shigella dysentery at an urban tertiary care center. All five patients presented with several days of bloody diarrhea. Stool culture was positive in one, PCR was positive in two, and blood cultures were positive in two. Of the identified subspecies (n=3), all were Shigella flexneri. Four of the five patients had active IV drug use, and one patient engaged in MSM. Two patients underwent colonoscopy, with significant inflammation extending throughout the colon, and into the terminal ileum in one case.
Two patients were empirically started on steroids after colonoscopy due to concern for IBD, however steroids were discontinued after identification of Shigella infection. One patient with bacteremia died, and the remaining 4 had resolution of their symptoms. Patients were treated with differing courses of antibiotics, including ertapenem for severe disease.
Discussion: Shigella is an important cause of infectious bloody diarrhea, and timely diagnosis is important on a personal and community level. The pattern of inflammation can mimic IBD, and our case series highlights more severe disease in patients with IV drug use (likely a proxy for malnutrition and poverty) and MSM. All identified strains were Shigella flexneri, which is less common than Shigella soneii although typically causes a more severe course; two of our patients had bacteremia. Only one of out the five cases was diagnosed based on stool culture. We observed inflammation into the ascending colon and TI, extending beyond what is typically seen in the rectosigmoid. Antibiotics are often reserved for patients who are immunocompromised or have severe disease, although there increasing drug resistance. Follow up testing is not required.
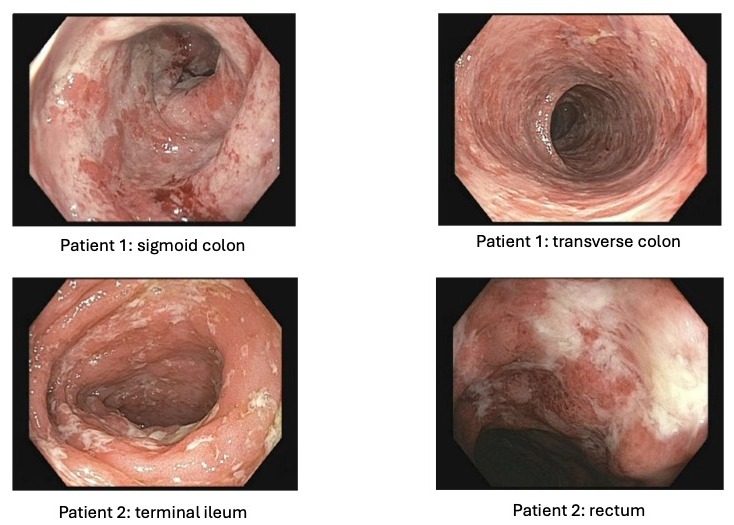
Figure: Endoscopic images
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Lindsay Matthews indicated no relevant financial relationships.
Christa Smaltz indicated no relevant financial relationships.
Holly Greenwald indicated no relevant financial relationships.
Lindsay Matthews, MD1, Christa Smaltz, MD1, Holly Greenwald, MD2. P0385 - An Outbreak of <i>Shigella</i> Dysentery at an Urban Tertiary Care Hospital, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
