Sunday Poster Session
Category: Colorectal Cancer Prevention
P0396 - Rates and Characteristics of Post-Polypectomy Interval Colorectal Cancer: A Single Center Retrospective Cohort Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Jacquelin Blomker, MD
University of Minnesota and Minneapolis VA Health Care System
Minneapolis, MN
Presenting Author(s)
Jacquelin Blomker, MD1, Tessa Herman, MD1, Rahul Karna, MD2, Michael Andreone, MD3, Mohammad Bilal, MD1
1University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3University of Minnesota, Minneapolis, MN
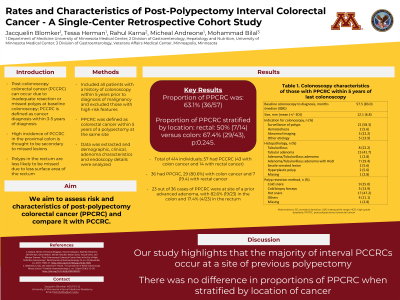
Introduction: Post-colonoscopy colorectal cancer (PCCRC) can occur due to missed polyps or incomplete polyp resection on initial colonoscopy. High incidence of PCCRC in the proximal colon is thought to be secondary to missed lesions and therefore a second look in the right side of colon is recommended. Polyps in the rectum are thought to be less likely missed due to less surface area of the rectum. Thus, we hypothesized that PCCRC in the rectum is more likely to occur due to incomplete polyp resection. We aimed to assess the risk and characteristics of post-polypectomy colorectal cancer.
Methods: We included all patients with colorectal cancer (CRC) who underwent a colonoscopy within 5 years prior to diagnosis of CRC at our institution from 2004-2023. PCCRC was defined as CRC (colorectal cancer) within 5 years of a colonoscopy. Patients who had CRC on initial colonoscopy or those with history of inflammatory bowel disease and familial polyposis syndromes were excluded from the analysis. Post-polypectomy colorectal cancer (PPCRC) was defined as CRC at the exact site of previous polypectomy within 5 years of a colonoscopy. Site of the previous polypectomy was confirmed by reviewing endoscopic images. Demographic, clinical, and adenoma characteristics as well as endoscopy details were analyzed and extracted. Our primary outcome was the rate of PPCRC. The secondary outcome was proportion of PPCRC stratified by location.
Results: Out of 414 cases of CRC diagnosed in the study period, 57 were PCCRC (43 with colon cancer and 14 with rectal cancer). 36 out of 57 had PPCRC (63.1%), with 80% (29/36) being colon cancer and 19.4% (7/36) rectal cancer. Table 1 shows demographics, colonoscopy, and pathology details of PPCRC. There was no difference in rates of PCCRC based on location (rectum 11.6% vs colon 13.7%, p=0.45). There was also no difference in proportion of PPCRC as stratified by location (rectum 50% (7/14) vs colon 67.4% (29/43), p:0.245). 23 out of 36 cases of PPCRC were at site of a prior advanced adenoma, with 82.6% (19/23) in the colon and 17.4% (4/23) in the rectum.
Discussion: Our study highlights that the majority of interval PCCRCs occur at a site of previous polypectomy. In addition, there was no difference in proportions of PPCRC when stratified by location of cancer. These findings reinforce the need for quality metrics focusing on polypectomy technique and careful inspection of polypectomy sites to assess for any residual polypoid tissue.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jacquelin Blomker, MD1, Tessa Herman, MD1, Rahul Karna, MD2, Michael Andreone, MD3, Mohammad Bilal, MD1. P0396 - Rates and Characteristics of Post-Polypectomy Interval Colorectal Cancer: A Single Center Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3University of Minnesota, Minneapolis, MN
Introduction: Post-colonoscopy colorectal cancer (PCCRC) can occur due to missed polyps or incomplete polyp resection on initial colonoscopy. High incidence of PCCRC in the proximal colon is thought to be secondary to missed lesions and therefore a second look in the right side of colon is recommended. Polyps in the rectum are thought to be less likely missed due to less surface area of the rectum. Thus, we hypothesized that PCCRC in the rectum is more likely to occur due to incomplete polyp resection. We aimed to assess the risk and characteristics of post-polypectomy colorectal cancer.
Methods: We included all patients with colorectal cancer (CRC) who underwent a colonoscopy within 5 years prior to diagnosis of CRC at our institution from 2004-2023. PCCRC was defined as CRC (colorectal cancer) within 5 years of a colonoscopy. Patients who had CRC on initial colonoscopy or those with history of inflammatory bowel disease and familial polyposis syndromes were excluded from the analysis. Post-polypectomy colorectal cancer (PPCRC) was defined as CRC at the exact site of previous polypectomy within 5 years of a colonoscopy. Site of the previous polypectomy was confirmed by reviewing endoscopic images. Demographic, clinical, and adenoma characteristics as well as endoscopy details were analyzed and extracted. Our primary outcome was the rate of PPCRC. The secondary outcome was proportion of PPCRC stratified by location.
Results: Out of 414 cases of CRC diagnosed in the study period, 57 were PCCRC (43 with colon cancer and 14 with rectal cancer). 36 out of 57 had PPCRC (63.1%), with 80% (29/36) being colon cancer and 19.4% (7/36) rectal cancer. Table 1 shows demographics, colonoscopy, and pathology details of PPCRC. There was no difference in rates of PCCRC based on location (rectum 11.6% vs colon 13.7%, p=0.45). There was also no difference in proportion of PPCRC as stratified by location (rectum 50% (7/14) vs colon 67.4% (29/43), p:0.245). 23 out of 36 cases of PPCRC were at site of a prior advanced adenoma, with 82.6% (19/23) in the colon and 17.4% (4/23) in the rectum.
Discussion: Our study highlights that the majority of interval PCCRCs occur at a site of previous polypectomy. In addition, there was no difference in proportions of PPCRC when stratified by location of cancer. These findings reinforce the need for quality metrics focusing on polypectomy technique and careful inspection of polypectomy sites to assess for any residual polypoid tissue.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jacquelin Blomker indicated no relevant financial relationships.
Tessa Herman indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Michael Andreone indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Speakers Bureau.
Jacquelin Blomker, MD1, Tessa Herman, MD1, Rahul Karna, MD2, Michael Andreone, MD3, Mohammad Bilal, MD1. P0396 - Rates and Characteristics of Post-Polypectomy Interval Colorectal Cancer: A Single Center Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
