Sunday Poster Session
Category: Colon
P0305 - A Postpolypectomy Syndrome Mimic Following Cold Snare
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Ryan Plunkett, MD
Saint Louis University School of Medicine
St. Louis, MO
Presenting Author(s)
Ryan Plunkett, MD1, Neel Matiwala, BS1, Matthew Schroeder, MD2, Hayden Rotramel, MD3, Jered Schenk, MD4, Ameya Deshmukh, DO1, Michael Presti, MD5
1Saint Louis University School of Medicine, St. Louis, MO; 2Washington University School of Medicine in St. Louis, St. Louis, MO; 3SSM Health Saint Louis University Hospital, St. Louis, MO; 4Medical University of South Carolina, Charleston, SC; 5St. Louis Veterans Affairs Medical Center, St. Louis, MO
Introduction: Postpolypectomy syndrome (PPS) presents with abdominal pain, leukocytosis, and localized peritonitis following colonoscopy with polypectomy. PPS has been attributed to hot snare polypectomy (HSP) as the electrocautery can lead to transmural thermal injury. We present a case mimicking PPS after cold snare and biopsy forceps polypectomy (CSP/CFP).
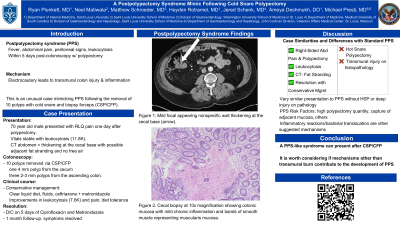
Case Description/Methods: A 70 year old male presented with localized, right lower quadrant pain without peritoneal signs one day after polypectomy. 10 polyps were removed via CSP/CFP notably with one 4 mm polyp from the cecum and three 2-3 mm polyps from the ascending colon. On admission, the patient was hemodynamically stable with leukocytosis (11.8K). CT of the abdomen showed nonspecific focal thickening at the cecal base with possible adjacent fat stranding and no free air or loculations. Although no electrocautery was used, the combination of a leukocytosis, abdominal pain, and mild cecal thickening following polypectomy posed concern for PPS. The patient was started on a clear liquid diet, isotonic fluids, ceftriaxone, and metronidazole with gastroenterology consultation. The next day, the patient was discharged on a 5 day course of ciprofloxacin and metronidazole after improvement in leukocytosis (7.6K) and pain, toleration of clear liquids, and passage of flatus. At 1 month follow up, the patient’s symptoms had resolved.
Discussion: PPS is currently understood as a reaction to transmural injury related to electrocautery. HSP more frequently obtains thicker samples than CSP. PPS also commonly occurs in the right colon due to its thinner wall. The similarity of symptoms in our case without HSP may question if the current pathophysiologic hypothesis fully addresses all causes of colonic injury. Only two other published cases describe PPS-like symptoms after cold interventions: 1) cold snare endoscopic mucosal resection of a 7-mm sessile serrated lesion requiring submucosal epinephrine injection and 2) CSP of fifty < 5-mm sessile, rectal polyps in a familial adenomatous polyposis patient. Connecting these cases by location, number of resections, and technique is difficult. More evidence is necessary to assess how the number of resections and histological depth from CSP/CFP affect local inflammation.
1.Hong HS, Yang DH, Postpolypectomy syndrome after cold snare endoscopic mucosal resection, 2022, 590-591.
2.Núñez-Pizarro JL, Luzko I, Rivero-Sánchez L, Postpolypectomy syndrome after multiple cold-snare polypectomies in the rectum, 2023, 928.

Disclosures:
Ryan Plunkett, MD1, Neel Matiwala, BS1, Matthew Schroeder, MD2, Hayden Rotramel, MD3, Jered Schenk, MD4, Ameya Deshmukh, DO1, Michael Presti, MD5. P0305 - A Postpolypectomy Syndrome Mimic Following Cold Snare, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Saint Louis University School of Medicine, St. Louis, MO; 2Washington University School of Medicine in St. Louis, St. Louis, MO; 3SSM Health Saint Louis University Hospital, St. Louis, MO; 4Medical University of South Carolina, Charleston, SC; 5St. Louis Veterans Affairs Medical Center, St. Louis, MO
Introduction: Postpolypectomy syndrome (PPS) presents with abdominal pain, leukocytosis, and localized peritonitis following colonoscopy with polypectomy. PPS has been attributed to hot snare polypectomy (HSP) as the electrocautery can lead to transmural thermal injury. We present a case mimicking PPS after cold snare and biopsy forceps polypectomy (CSP/CFP).
Case Description/Methods: A 70 year old male presented with localized, right lower quadrant pain without peritoneal signs one day after polypectomy. 10 polyps were removed via CSP/CFP notably with one 4 mm polyp from the cecum and three 2-3 mm polyps from the ascending colon. On admission, the patient was hemodynamically stable with leukocytosis (11.8K). CT of the abdomen showed nonspecific focal thickening at the cecal base with possible adjacent fat stranding and no free air or loculations. Although no electrocautery was used, the combination of a leukocytosis, abdominal pain, and mild cecal thickening following polypectomy posed concern for PPS. The patient was started on a clear liquid diet, isotonic fluids, ceftriaxone, and metronidazole with gastroenterology consultation. The next day, the patient was discharged on a 5 day course of ciprofloxacin and metronidazole after improvement in leukocytosis (7.6K) and pain, toleration of clear liquids, and passage of flatus. At 1 month follow up, the patient’s symptoms had resolved.
Discussion: PPS is currently understood as a reaction to transmural injury related to electrocautery. HSP more frequently obtains thicker samples than CSP. PPS also commonly occurs in the right colon due to its thinner wall. The similarity of symptoms in our case without HSP may question if the current pathophysiologic hypothesis fully addresses all causes of colonic injury. Only two other published cases describe PPS-like symptoms after cold interventions: 1) cold snare endoscopic mucosal resection of a 7-mm sessile serrated lesion requiring submucosal epinephrine injection and 2) CSP of fifty < 5-mm sessile, rectal polyps in a familial adenomatous polyposis patient. Connecting these cases by location, number of resections, and technique is difficult. More evidence is necessary to assess how the number of resections and histological depth from CSP/CFP affect local inflammation.
1.Hong HS, Yang DH, Postpolypectomy syndrome after cold snare endoscopic mucosal resection, 2022, 590-591.
2.Núñez-Pizarro JL, Luzko I, Rivero-Sánchez L, Postpolypectomy syndrome after multiple cold-snare polypectomies in the rectum, 2023, 928.

Figure: Figure 1: CT abdomen-pelvis demonstrating mild, focal appearing, nonspecific wall thickening at the cecal base after polypectomy.
Disclosures:
Ryan Plunkett indicated no relevant financial relationships.
Neel Matiwala indicated no relevant financial relationships.
Matthew Schroeder indicated no relevant financial relationships.
Hayden Rotramel indicated no relevant financial relationships.
Jered Schenk indicated no relevant financial relationships.
Ameya Deshmukh indicated no relevant financial relationships.
Michael Presti indicated no relevant financial relationships.
Ryan Plunkett, MD1, Neel Matiwala, BS1, Matthew Schroeder, MD2, Hayden Rotramel, MD3, Jered Schenk, MD4, Ameya Deshmukh, DO1, Michael Presti, MD5. P0305 - A Postpolypectomy Syndrome Mimic Following Cold Snare, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

