Sunday Poster Session
Category: Colon
P0308 - Atypical Presentation of Rectal Bleeding: Unveiling Severe Proctosigmoiditis and Concurrent HIV, Syphilis, Gonorrhea, and Chlamydia Infections
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- WD
William Davis, DO
Henry Ford Health
Madison Heights, MI
Presenting Author(s)
William Davis, DO1, Syed Ahmad Adil, MD2, Adarsh K. Varma, MD2, Amit Bhan, MD3
1Henry Ford Health, Madison Heights, MI; 2Henry Ford Health, Detroit, MI; 3Henry Ford Hospital, Detroit, MI
Introduction: Proctitis is defined as inflammation involving the distal rectum. The presenting symptoms can be non-specific, thus takes a careful history and diagnostic work-up for diagnosis and management. We present a case of a 30-year-old male presenting for hematochezia and rectal pain initially attributed to hemorrhoids; however, diagnostic work-up led to diagnosis of infectious proctitis.
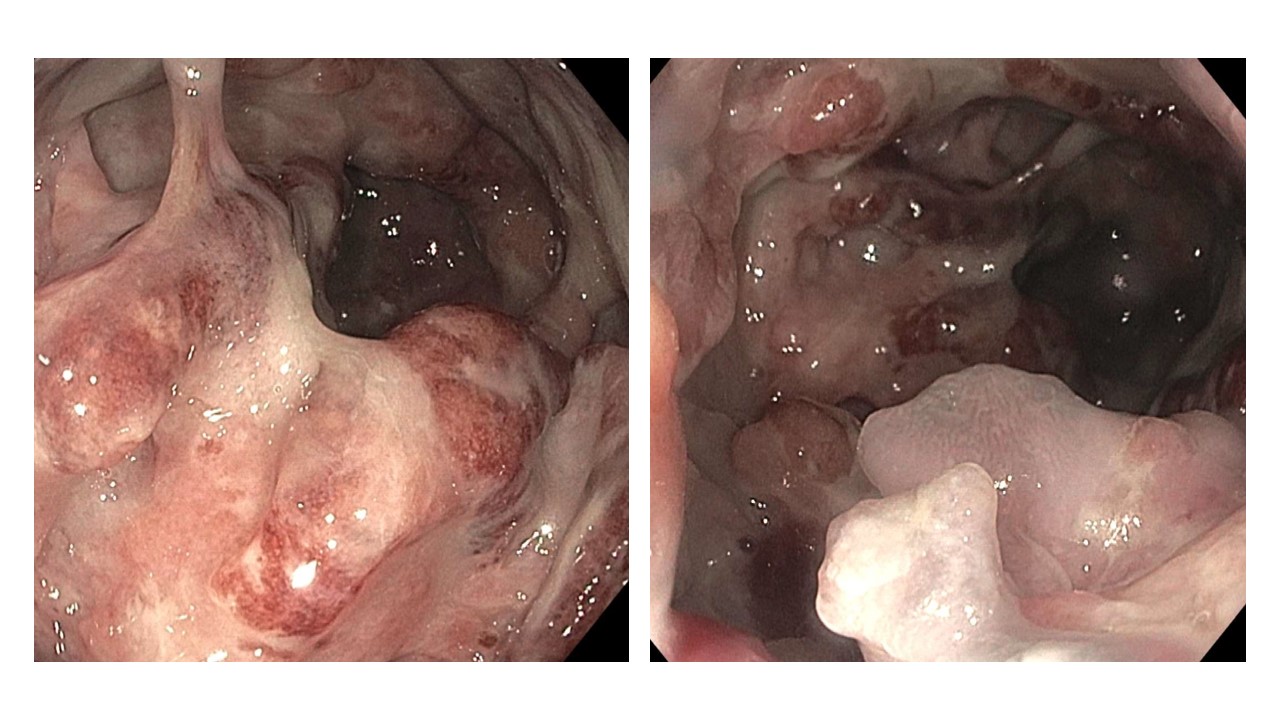
Case Description/Methods: A 30-year-old previously healthy male presented to the emergency department with a two-month history of painful rectal bleeding, initially attributed to hemorrhoids on outpatient work up. The severity of his pain led to fear of defecation, food aversion, and a 30-pound weight loss. Despite laxatives, topical creams, and Sitz baths, he found no relief. Upon assessment, he exhibited diaphoresis and tachycardia. Initial hemoglobin levels revealed a significant drop from his baseline of 13 g/dL to 7.5 g/dL. A rectal examination elicited pain and identified a small external hemorrhoid. Colonoscopy was performed for further evaluation and revealed multiple ulcerated, violaceous, and erythematous plaques from the anal verge to 20 cm and multiple perianal condylomas. Rectal biopsies were taken, revealing severe active proctitis. Due to suspicion of sexually transmitted infections, infectious work up was completed showing positive for HIV (CD4 count: 553, viral load: 85,000), syphilis, along with positive gonorrhea and chlamydia lymphogranuloma venereum (LGV). On further history, he reported multiple sexual partners, including men and women that was previously denied. Infectious disease consultation led to initiation of antiretroviral therapy and treatment for syphilis, gonorrhea, and chlamydia. A month after admission, the viral load was undetectable, and hemoglobin levels had risen to 11 g/dL. Patients rectal bleeding had resolved, however continues to report significant rectal pain one month after diagnosis.
Discussion: As seen in this case, the diagnosis of proctitis can often be delayed and can result in significant patient distress. Our patient’s endoscopic findings were consistent with long standing LGV, characterized by diffuse granulomatous lesions. As with our patient, co-infection can often be seen in concomitant HIV. Thus, patients with suspicion of infectious proctitis should have a detailed infectious work up to ensure complete treatment. This emphasizes the importance of a thorough history to guide diagnostic work up for prompt diagnosis and treatment.
Disclosures:
William Davis, DO1, Syed Ahmad Adil, MD2, Adarsh K. Varma, MD2, Amit Bhan, MD3. P0308 - Atypical Presentation of Rectal Bleeding: Unveiling Severe Proctosigmoiditis and Concurrent HIV, Syphilis, Gonorrhea, and Chlamydia Infections, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Health, Madison Heights, MI; 2Henry Ford Health, Detroit, MI; 3Henry Ford Hospital, Detroit, MI
Introduction: Proctitis is defined as inflammation involving the distal rectum. The presenting symptoms can be non-specific, thus takes a careful history and diagnostic work-up for diagnosis and management. We present a case of a 30-year-old male presenting for hematochezia and rectal pain initially attributed to hemorrhoids; however, diagnostic work-up led to diagnosis of infectious proctitis.
Case Description/Methods: A 30-year-old previously healthy male presented to the emergency department with a two-month history of painful rectal bleeding, initially attributed to hemorrhoids on outpatient work up. The severity of his pain led to fear of defecation, food aversion, and a 30-pound weight loss. Despite laxatives, topical creams, and Sitz baths, he found no relief. Upon assessment, he exhibited diaphoresis and tachycardia. Initial hemoglobin levels revealed a significant drop from his baseline of 13 g/dL to 7.5 g/dL. A rectal examination elicited pain and identified a small external hemorrhoid. Colonoscopy was performed for further evaluation and revealed multiple ulcerated, violaceous, and erythematous plaques from the anal verge to 20 cm and multiple perianal condylomas. Rectal biopsies were taken, revealing severe active proctitis. Due to suspicion of sexually transmitted infections, infectious work up was completed showing positive for HIV (CD4 count: 553, viral load: 85,000), syphilis, along with positive gonorrhea and chlamydia lymphogranuloma venereum (LGV). On further history, he reported multiple sexual partners, including men and women that was previously denied. Infectious disease consultation led to initiation of antiretroviral therapy and treatment for syphilis, gonorrhea, and chlamydia. A month after admission, the viral load was undetectable, and hemoglobin levels had risen to 11 g/dL. Patients rectal bleeding had resolved, however continues to report significant rectal pain one month after diagnosis.
Discussion: As seen in this case, the diagnosis of proctitis can often be delayed and can result in significant patient distress. Our patient’s endoscopic findings were consistent with long standing LGV, characterized by diffuse granulomatous lesions. As with our patient, co-infection can often be seen in concomitant HIV. Thus, patients with suspicion of infectious proctitis should have a detailed infectious work up to ensure complete treatment. This emphasizes the importance of a thorough history to guide diagnostic work up for prompt diagnosis and treatment.
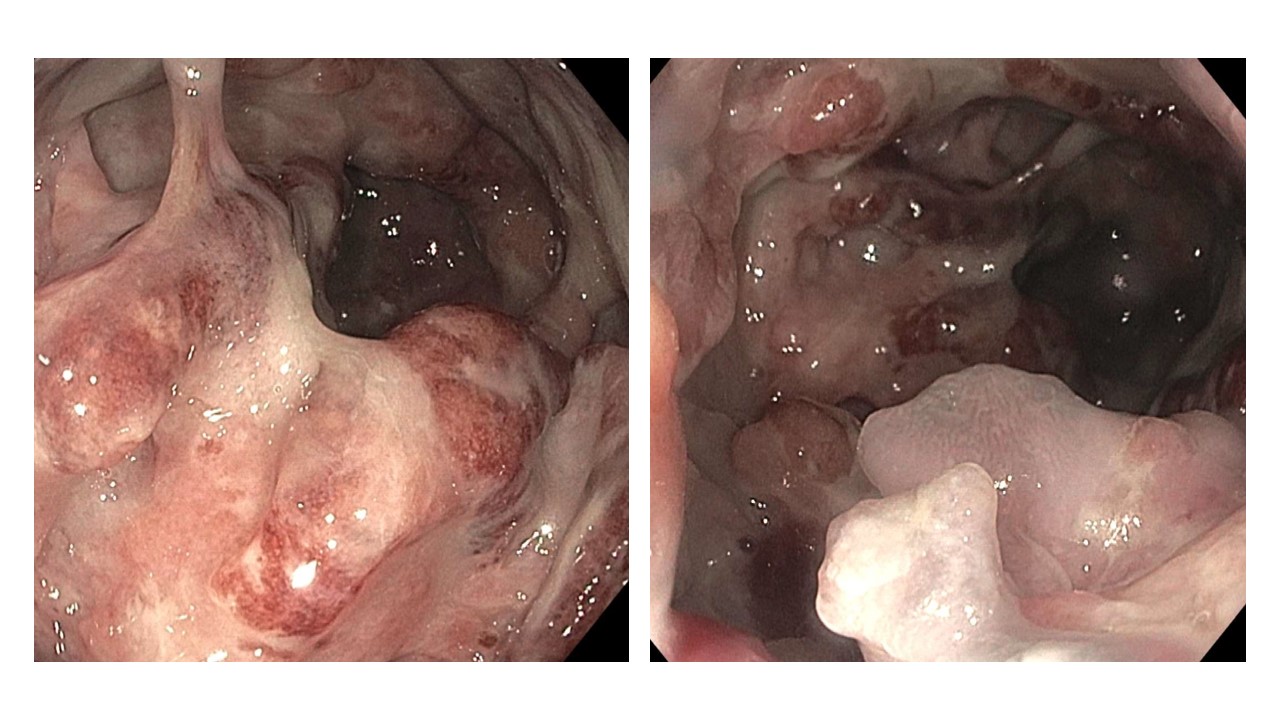
Figure: Endoscopic visualization of purple violaceous erythematous plaques with large ulcerations in the rectum and sigmoid colon.
Disclosures:
William Davis indicated no relevant financial relationships.
Syed Ahmad Adil indicated no relevant financial relationships.
Adarsh Varma indicated no relevant financial relationships.
Amit Bhan indicated no relevant financial relationships.
William Davis, DO1, Syed Ahmad Adil, MD2, Adarsh K. Varma, MD2, Amit Bhan, MD3. P0308 - Atypical Presentation of Rectal Bleeding: Unveiling Severe Proctosigmoiditis and Concurrent HIV, Syphilis, Gonorrhea, and Chlamydia Infections, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
