Sunday Poster Session
Category: Colon
P0309 - Malakoplakia Mimicking Metastatic Colon Cancer
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- WD
William Davis, DO
Henry Ford Health
Madison Heights, MI
Presenting Author(s)
William Davis, DO1, Bipneet Singh, MBBS2, Anas Kutait, MD3, Omar Abbas, MD3
1Henry Ford Health, Madison Heights, MI; 2Henry Ford Jackson Hospital, Detroit, MI; 3Henry Ford Health, Detroit, MI
Introduction: Malakoplakia is a rare, chronic granulomatous inflammatory disease that results from impaired histiocyte clearance of bacteria in immune compromised individuals. We present a case of a post-lung transplant patient that was suspected to have diffuse colonic metastatic disease based on computed tomography (CT) that was later deemed to be diffuse malakoplakia related to systemic infection.
Case Description/Methods: A 62-year-old female with history of lung transplant on Tacrolimus presented with abdominal distension and diarrhea. Vital signs were stable on arrival. Laboratory results including a complete blood count, liver and chemistry panels were noncontributory. Blood cultures repetitively grew Achromobacter xylosoxidans despite escalation of antibiotic therapy. Abdominal and pelvic CT demonstrated gastric distension, and a colonic filling defect at the hepatic flexure with extensive adenopathy evading the duodenal serosa. At this time there were concerns of metastatic colon cancer with concomitant systemic infection.
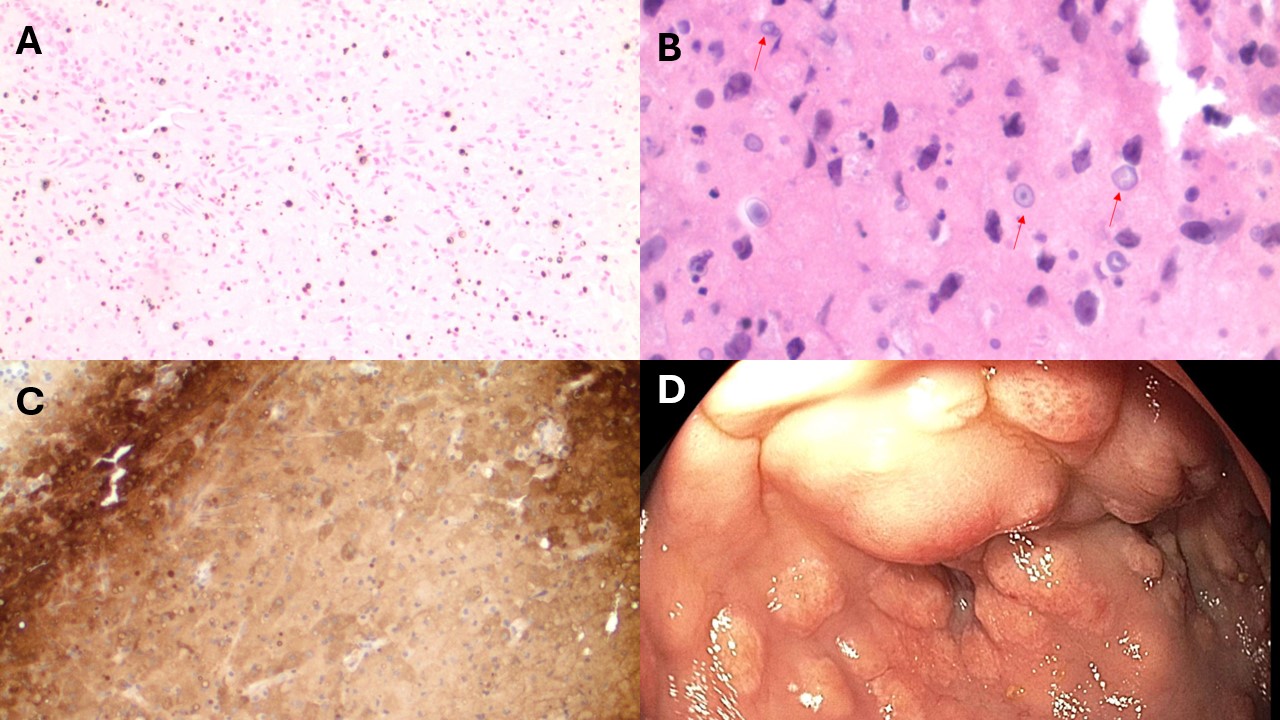
Interventional radiology performed lymph node biopsy revealing malakoplakia and negative for malignancy. Multidisciplinary discussion between infectious disease and gastroenterology was performed with concerns for the colonic filling defect as the origin of patient's persistent bacteremia. Colonoscopy was performed showing diffuse nodularity with ulcerations encompassing the right colon without a targetable lesion for source control. Biopsies were obtained redemonstrating malakoplakia. The patient’s hospital course was complicated by COVID-19 pneumonia and ultimately expiring due to respiratory failure.
Discussion: Malakoplakia is a poorly understood and rare chronic granulomatous inflammatory disease that results from bactericidal defect of histiocytes. This manifests in an accumulation of phagolysosomes most commonly in immune compromised individuals. Symptoms are non-specific ranging from asymptomatic to altered bowel habits, abdominal pain, rectal bleeding, and intestinal obstruction. Endoscopic appearance can range from flat lesions to multiple ulcerated polypoid nodules. Thus, as in this case, the diagnosis can often be delayed and result in unnecessary interventions until a true diagnosis is achieved. Once diagnosed antibiotic therapy is tailored to the culprit organism resulting an accumulation within histiocytes and killing the bacteria. This case serves to educate the reader of this rare disease presentation to limit extensive work up and expedite treatment.
Disclosures:
William Davis, DO1, Bipneet Singh, MBBS2, Anas Kutait, MD3, Omar Abbas, MD3. P0309 - Malakoplakia Mimicking Metastatic Colon Cancer, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Health, Madison Heights, MI; 2Henry Ford Jackson Hospital, Detroit, MI; 3Henry Ford Health, Detroit, MI
Introduction: Malakoplakia is a rare, chronic granulomatous inflammatory disease that results from impaired histiocyte clearance of bacteria in immune compromised individuals. We present a case of a post-lung transplant patient that was suspected to have diffuse colonic metastatic disease based on computed tomography (CT) that was later deemed to be diffuse malakoplakia related to systemic infection.
Case Description/Methods: A 62-year-old female with history of lung transplant on Tacrolimus presented with abdominal distension and diarrhea. Vital signs were stable on arrival. Laboratory results including a complete blood count, liver and chemistry panels were noncontributory. Blood cultures repetitively grew Achromobacter xylosoxidans despite escalation of antibiotic therapy. Abdominal and pelvic CT demonstrated gastric distension, and a colonic filling defect at the hepatic flexure with extensive adenopathy evading the duodenal serosa. At this time there were concerns of metastatic colon cancer with concomitant systemic infection.
Interventional radiology performed lymph node biopsy revealing malakoplakia and negative for malignancy. Multidisciplinary discussion between infectious disease and gastroenterology was performed with concerns for the colonic filling defect as the origin of patient's persistent bacteremia. Colonoscopy was performed showing diffuse nodularity with ulcerations encompassing the right colon without a targetable lesion for source control. Biopsies were obtained redemonstrating malakoplakia. The patient’s hospital course was complicated by COVID-19 pneumonia and ultimately expiring due to respiratory failure.
Discussion: Malakoplakia is a poorly understood and rare chronic granulomatous inflammatory disease that results from bactericidal defect of histiocytes. This manifests in an accumulation of phagolysosomes most commonly in immune compromised individuals. Symptoms are non-specific ranging from asymptomatic to altered bowel habits, abdominal pain, rectal bleeding, and intestinal obstruction. Endoscopic appearance can range from flat lesions to multiple ulcerated polypoid nodules. Thus, as in this case, the diagnosis can often be delayed and result in unnecessary interventions until a true diagnosis is achieved. Once diagnosed antibiotic therapy is tailored to the culprit organism resulting an accumulation within histiocytes and killing the bacteria. This case serves to educate the reader of this rare disease presentation to limit extensive work up and expedite treatment.
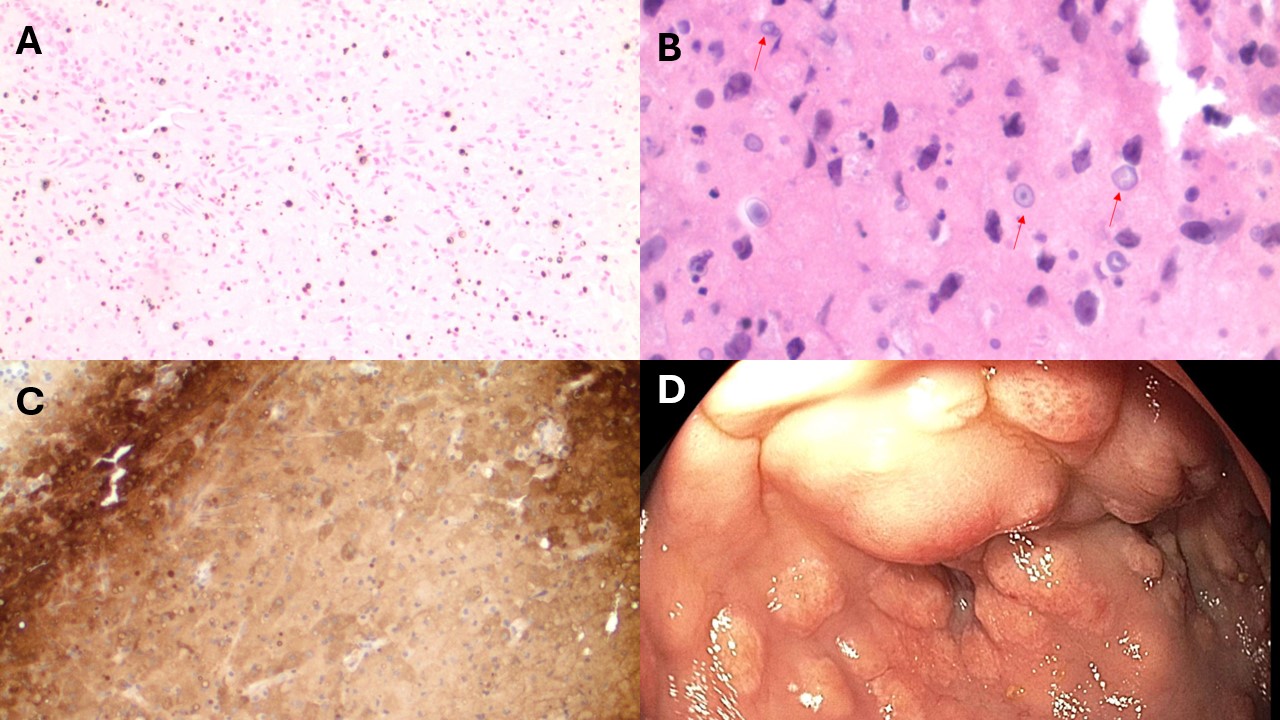
Figure: A) Ascending colon biopsy section, Von Kossa Stain: Calcium deposits within Michaelis-Guttman bodies are highlighted. B) Ascending colon biopsy section, Hematoxylin and Eosin stain (high magnification): Characteristic Michaelis-Guttman bodies (red arrows) are identified within the submucosal histiocytic infiltrate. C) Ascending colon biopsy section, CD68 immunohistochemical stain (high magnification): CD68 highlights the histiocytic infiltrate. Multiple Michaelis-Gutmann bodies are seen. D) Endoscopic visualization of nodular mucosa with ulcerations of the ascending colon.
Disclosures:
William Davis indicated no relevant financial relationships.
Bipneet Singh indicated no relevant financial relationships.
Anas Kutait indicated no relevant financial relationships.
Omar Abbas indicated no relevant financial relationships.
William Davis, DO1, Bipneet Singh, MBBS2, Anas Kutait, MD3, Omar Abbas, MD3. P0309 - Malakoplakia Mimicking Metastatic Colon Cancer, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
