Sunday Poster Session
Category: Colon
P0317 - Intestinal Spirochetosis: Commensal or Culprit?
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Amanda Frondella, MD
UConn John Dempsey Hospital
Farmington, CT
Presenting Author(s)
Amanda Frondella, MD1, Rohit Singhania, MBBS, MS2
1UConn John Dempsey Hospital, Farmington, CT; 2Connecticut GI, Manchester, CT
Introduction: Intestinal spirochetosis (IS) is a rare entity in the developed world, with a prevalence of 1.1 to 5%. It remains poorly understood and presents with varying signs and symptoms. It is caused by the gram-negative spirochete Brachyspira aalborgi. There has yet to be an agreement on the need, or lack thereof, for treatment. We present a case of IS in the setting of multiple gastrointestinal (GI) symptoms and an otherwise negative infectious and inflammatory workup.
Case Description/Methods: A 38-year-old immunocompetent male with history of gastroesophageal reflux disease returned to the US after living in Italy for 8 years and presented with 2 months of non-bloody diarrhea. Stools were reported to be Bristol 6, occurring 2-3 times daily. Of note, patient was treated with mebendazole in Italy 2 months prior for a presumed parasitic infection after he noted worms in his stool, accompanied by 4 weeks of abdominal pain, loss of appetite and a 35-pound weight loss. While in Italy he went on multiple camping trips in the mountains. Since returning to the US, comprehensive stool tests were negative for bacterial or parasitic infection. Stool calprotectin and pancreatic elastase-1 were within normal range. HIV testing was negative.
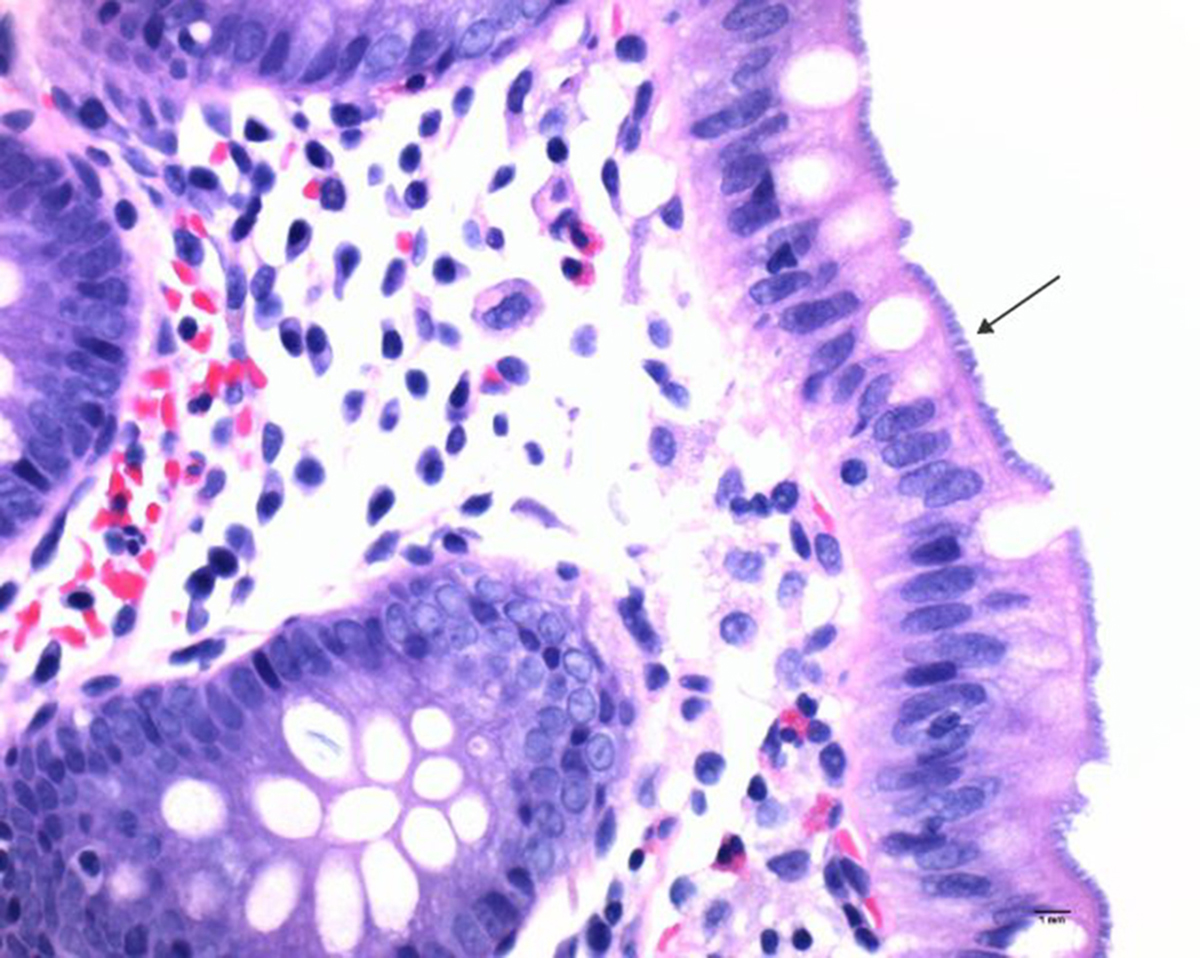
His weight had stabilized, however daily diarrheal episodes were increasing. Colonoscopy showed diverticulosis in the sigmoid and descending colon. Pathology showed a thin, dense layer of noninvasive spirochetes attached to the colonic luminal epithelium with no apparent reaction in the epithelium or subjacent stroma (Figure 1) – consistent with intestinal spirochetosis. The patient was advised to begin metronidazole and is planned for follow up to assess for resolution of symptoms.
Discussion: Intestinal spirochetosis is an uncommon finding, although its prevalence increases to 54% in homosexual men and HIV-positive individuals. Spirochetemia and multiple organ failure have been reported in critically ill patients with IS. Patients present with diverse GI symptoms and colonoscopy findings are subtle or absent. The appearance of a “false brush border” is a histological hallmark of this entity.
Whether or not IS is the cause of GI symptoms in immunocompetent patients is largely debated, as is the need for treatment. This is primarily because it has been an incidental finding in some individuals. Metronidazole is currently the preferred antibiotic treatment. This case highlights the paucity of literature on the topic and the need for further research and guideline development.
Disclosures:
Amanda Frondella, MD1, Rohit Singhania, MBBS, MS2. P0317 - Intestinal Spirochetosis: Commensal or Culprit?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1UConn John Dempsey Hospital, Farmington, CT; 2Connecticut GI, Manchester, CT
Introduction: Intestinal spirochetosis (IS) is a rare entity in the developed world, with a prevalence of 1.1 to 5%. It remains poorly understood and presents with varying signs and symptoms. It is caused by the gram-negative spirochete Brachyspira aalborgi. There has yet to be an agreement on the need, or lack thereof, for treatment. We present a case of IS in the setting of multiple gastrointestinal (GI) symptoms and an otherwise negative infectious and inflammatory workup.
Case Description/Methods: A 38-year-old immunocompetent male with history of gastroesophageal reflux disease returned to the US after living in Italy for 8 years and presented with 2 months of non-bloody diarrhea. Stools were reported to be Bristol 6, occurring 2-3 times daily. Of note, patient was treated with mebendazole in Italy 2 months prior for a presumed parasitic infection after he noted worms in his stool, accompanied by 4 weeks of abdominal pain, loss of appetite and a 35-pound weight loss. While in Italy he went on multiple camping trips in the mountains. Since returning to the US, comprehensive stool tests were negative for bacterial or parasitic infection. Stool calprotectin and pancreatic elastase-1 were within normal range. HIV testing was negative.
His weight had stabilized, however daily diarrheal episodes were increasing. Colonoscopy showed diverticulosis in the sigmoid and descending colon. Pathology showed a thin, dense layer of noninvasive spirochetes attached to the colonic luminal epithelium with no apparent reaction in the epithelium or subjacent stroma (Figure 1) – consistent with intestinal spirochetosis. The patient was advised to begin metronidazole and is planned for follow up to assess for resolution of symptoms.
Discussion: Intestinal spirochetosis is an uncommon finding, although its prevalence increases to 54% in homosexual men and HIV-positive individuals. Spirochetemia and multiple organ failure have been reported in critically ill patients with IS. Patients present with diverse GI symptoms and colonoscopy findings are subtle or absent. The appearance of a “false brush border” is a histological hallmark of this entity.
Whether or not IS is the cause of GI symptoms in immunocompetent patients is largely debated, as is the need for treatment. This is primarily because it has been an incidental finding in some individuals. Metronidazole is currently the preferred antibiotic treatment. This case highlights the paucity of literature on the topic and the need for further research and guideline development.
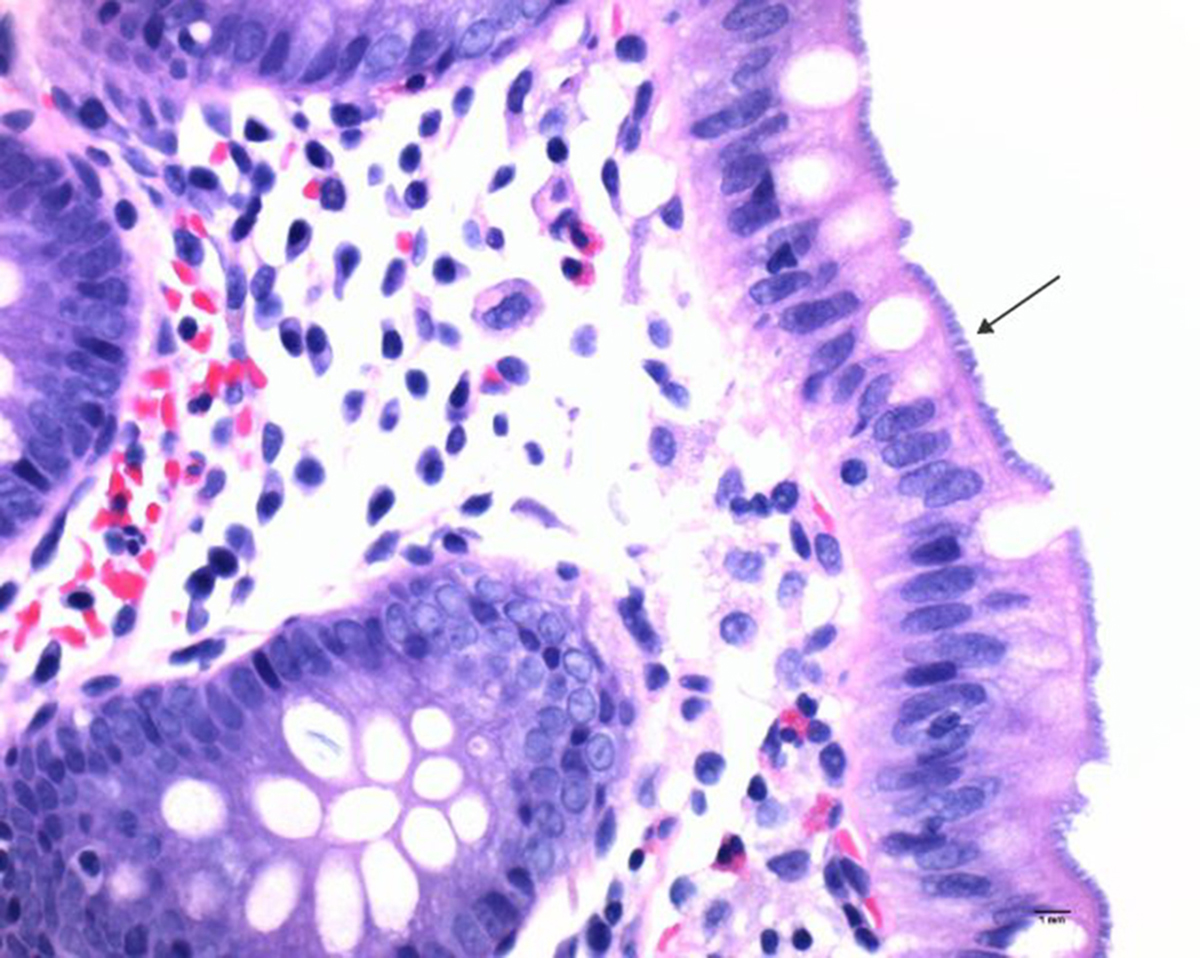
Figure: Figure 1. Colonoscopic biopsies showed a thin, dense layer of noninvasive spirochetes attached to the colonic luminal epithelium with no apparent reaction in the epithelium or subjacent stroma.
Disclosures:
Amanda Frondella indicated no relevant financial relationships.
Rohit Singhania: Phathom pharmaceuticals – Speakers Bureau.
Amanda Frondella, MD1, Rohit Singhania, MBBS, MS2. P0317 - Intestinal Spirochetosis: Commensal or Culprit?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
