Sunday Poster Session
Category: Colon
P0224 - Does Alcohol Use Impact Outcomes of Ischemic Colitis? A Retrospective Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rakahn Haddadin, MD
MountainView Hospital
Las Vegas, NV
Presenting Author(s)
Humzah Iqbal, MD1, Rakahn Haddadin, MD2, Fatimah Aftab, BS3, Hussein Riza, BS4, Hasib Haidary, BS5, Patrick Zhang, BS6, Haroon Iqbal, BS4, Devang Prajapati, MD1
1University of California San Francisco, Fresno, CA; 2MountainView Hospital, Las Vegas, NV; 3University of Toledo College of Medicine and Life Sciences, Toledo, OH; 4St. George's University, Irvine, CA; 5American University of Antigua, Irvine, CA; 6California Health Sciences University, Fresno, CA
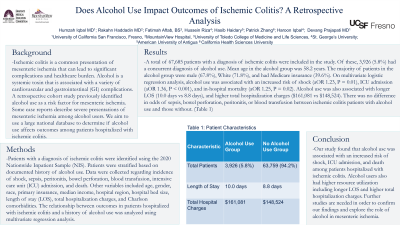
Introduction: Ischemic colitis is a common presentation of mesenteric ischemia that can lead to significant complications and healthcare burden. Alcohol is a systemic toxin that is associated with a variety of cardiovascular and gastrointestinal (GI) complications. A retrospective cohort study previously identified alcohol use as a risk factor for mesenteric ischemia. Some case reports describe severe presentations of mesenteric ischemia among alcohol users. We aim to use a large national database to determine if alcohol use affects outcomes among patients hospitalized with ischemic colitis.
Methods: Patients with a diagnosis of ischemic colitis were identified using the 2020 Nationwide Inpatient Sample (NIS). Patients were stratified based on documented history of alcohol use. Data were collected regarding incidence of shock, sepsis, peritonitis, bowel perforation, blood transfusion, intensive care unit (ICU) admission, and death. Other variables included age, gender, race, primary insurance, median income, hospital region, hospital bed size, length of stay (LOS), total hospitalization charges, and Charlson comorbidities. The relationship between outcomes in patients hospitalized with ischemic colitis and a history of alcohol use was analyzed using multivariate regression analysis.
Results: A total of 67,685 patients with a diagnosis of ischemic colitis were included in the study. Of these, 3,926 (5.8%) had a concurrent diagnosis of alcohol use. Mean age in the alcohol group was 58.2 years. The majority of patients in the alcohol group were male (67.8%), White (71.8%), and had Medicare insurance (39.6%). On multivariate logistic regression analysis, alcohol use was associated with an increased risk of shock (aOR 1.23, P = 0.01), ICU admission (aOR 1.36, P < 0.001), and in-hospital mortality (aOR 1.25, P = 0.02). Alcohol use was also associated with longer LOS (10.0 days vs 8.8 days), and higher total hospitalization charges ($161,081 vs $148,524). There was no difference in odds of sepsis, bowel perforation, peritonitis, or blood transfusion between ischemic colitis patients with alcohol use and those without.
Discussion: Our study found that alcohol use was associated with an increased risk of shock, ICU admission, and death among patients hospitalized with ischemic colitis. Alcohol users also had higher resource utilization including longer LOS and higher total hospitalization charges. Further studies are needed in order to confirm our findings and explore the role of alcohol in mesenteric ischemia.
Disclosures:
Humzah Iqbal, MD1, Rakahn Haddadin, MD2, Fatimah Aftab, BS3, Hussein Riza, BS4, Hasib Haidary, BS5, Patrick Zhang, BS6, Haroon Iqbal, BS4, Devang Prajapati, MD1. P0224 - Does Alcohol Use Impact Outcomes of Ischemic Colitis? A Retrospective Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of California San Francisco, Fresno, CA; 2MountainView Hospital, Las Vegas, NV; 3University of Toledo College of Medicine and Life Sciences, Toledo, OH; 4St. George's University, Irvine, CA; 5American University of Antigua, Irvine, CA; 6California Health Sciences University, Fresno, CA
Introduction: Ischemic colitis is a common presentation of mesenteric ischemia that can lead to significant complications and healthcare burden. Alcohol is a systemic toxin that is associated with a variety of cardiovascular and gastrointestinal (GI) complications. A retrospective cohort study previously identified alcohol use as a risk factor for mesenteric ischemia. Some case reports describe severe presentations of mesenteric ischemia among alcohol users. We aim to use a large national database to determine if alcohol use affects outcomes among patients hospitalized with ischemic colitis.
Methods: Patients with a diagnosis of ischemic colitis were identified using the 2020 Nationwide Inpatient Sample (NIS). Patients were stratified based on documented history of alcohol use. Data were collected regarding incidence of shock, sepsis, peritonitis, bowel perforation, blood transfusion, intensive care unit (ICU) admission, and death. Other variables included age, gender, race, primary insurance, median income, hospital region, hospital bed size, length of stay (LOS), total hospitalization charges, and Charlson comorbidities. The relationship between outcomes in patients hospitalized with ischemic colitis and a history of alcohol use was analyzed using multivariate regression analysis.
Results: A total of 67,685 patients with a diagnosis of ischemic colitis were included in the study. Of these, 3,926 (5.8%) had a concurrent diagnosis of alcohol use. Mean age in the alcohol group was 58.2 years. The majority of patients in the alcohol group were male (67.8%), White (71.8%), and had Medicare insurance (39.6%). On multivariate logistic regression analysis, alcohol use was associated with an increased risk of shock (aOR 1.23, P = 0.01), ICU admission (aOR 1.36, P < 0.001), and in-hospital mortality (aOR 1.25, P = 0.02). Alcohol use was also associated with longer LOS (10.0 days vs 8.8 days), and higher total hospitalization charges ($161,081 vs $148,524). There was no difference in odds of sepsis, bowel perforation, peritonitis, or blood transfusion between ischemic colitis patients with alcohol use and those without.
Discussion: Our study found that alcohol use was associated with an increased risk of shock, ICU admission, and death among patients hospitalized with ischemic colitis. Alcohol users also had higher resource utilization including longer LOS and higher total hospitalization charges. Further studies are needed in order to confirm our findings and explore the role of alcohol in mesenteric ischemia.
Disclosures:
Humzah Iqbal indicated no relevant financial relationships.
Rakahn Haddadin indicated no relevant financial relationships.
Fatimah Aftab indicated no relevant financial relationships.
Hussein Riza indicated no relevant financial relationships.
Hasib Haidary indicated no relevant financial relationships.
Patrick Zhang indicated no relevant financial relationships.
Haroon Iqbal indicated no relevant financial relationships.
Devang Prajapati indicated no relevant financial relationships.
Humzah Iqbal, MD1, Rakahn Haddadin, MD2, Fatimah Aftab, BS3, Hussein Riza, BS4, Hasib Haidary, BS5, Patrick Zhang, BS6, Haroon Iqbal, BS4, Devang Prajapati, MD1. P0224 - Does Alcohol Use Impact Outcomes of Ischemic Colitis? A Retrospective Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
