Sunday Poster Session
Category: Biliary/Pancreas
P0149 - From Bile to Brain: Paraneoplastic Cerebellar Degeneration In Cholangiocarcinoma
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- AK
Adam Khalaf, MD
MedStar Georgetown University Hospital
Washington, Canada
Presenting Author(s)
Adam Khalaf, MD, Sravya Jannapureddy, MD, Harjit Singh, MD, MBA, Carl Sun, MD, Lydia Bunker, MD
MedStar Georgetown University Hospital, Washington, DC
Introduction: Intrahepatic cholangiocarcinoma (iCCA) is an epithelial malignancy with increasing incidence (annual percentage change 4.6%) and high mortality rates due to atypical presentations and late-stage diagnosis. Paraneoplastic syndromes in cholangiocarcinoma (CCA) are extremely rare, affect multiple organ systems, and involve dysfunctional immune responses. We present the case of a 76-year-old man with a liver lesion and neurological symptoms suggestive of acute paraneoplastic cerebellar degeneration (PCD), later diagnosed with iCCA.
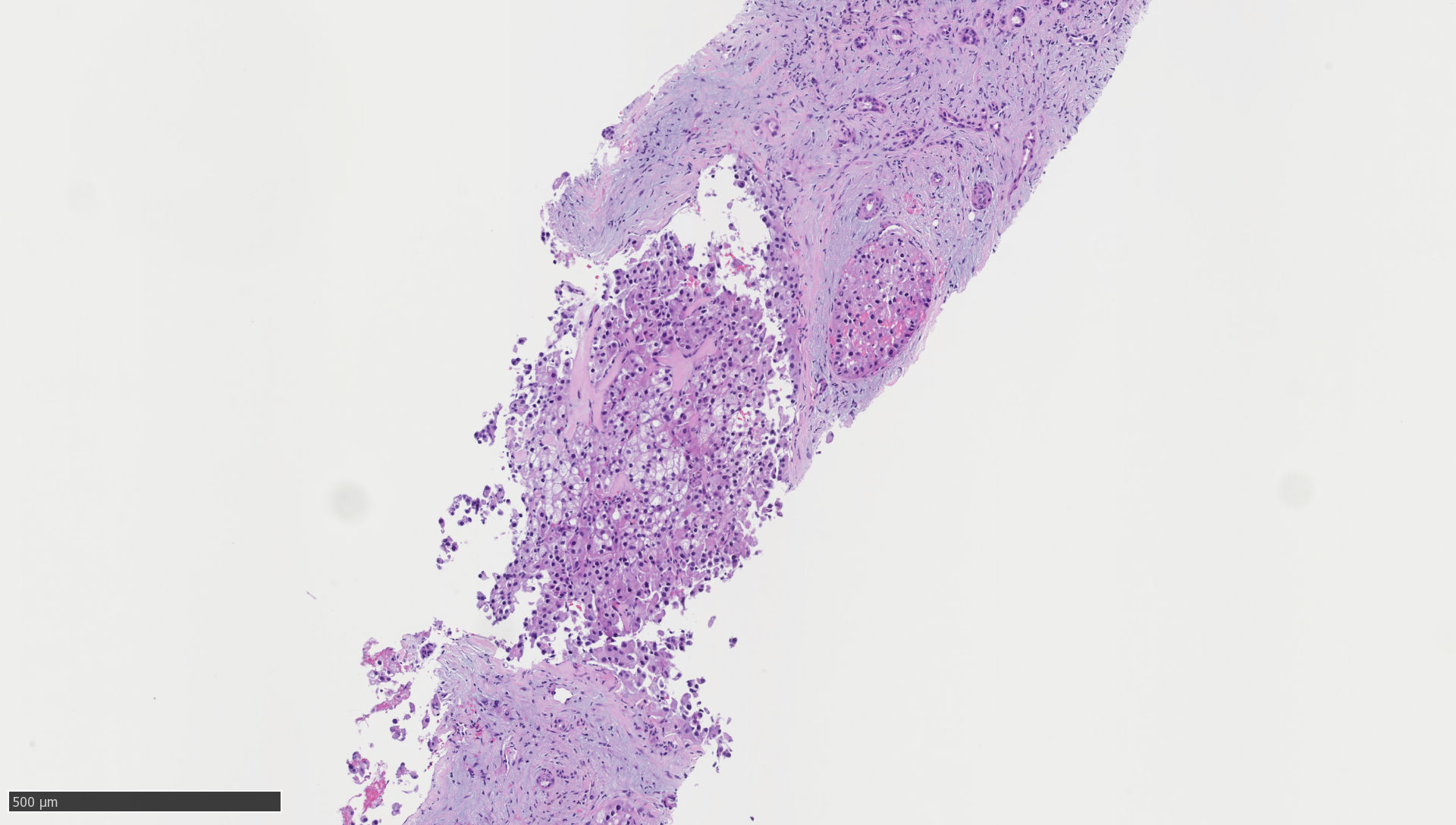
Case Description/Methods: A 76-year-old male with a history of multiple myeloma, ischemic stroke, and type II diabetes presented with a 2-month history of progressive lower extremity (LE) weakness that had recently worsened, rendering him bedridden. Physical exam revealed dysarthria and diminished strength with delayed reflexes in his bilateral LE. Pan-CT imaging revealed a chronic infarct of the middle cerebral artery and an indeterminate liver lesion measuring 5.2 × 3.7 cm in segment 4 of the left hepatic lobe. One-week after admission, he developed bulbar dysphagia and tongue fasciculations. Liver enzymes were normal on arrival but peaked at AST 119 and ALT 134 nine days later. Cerebrospinal fluid (CSF) testing revealed slightly elevated glucose (80) and IgG index (0.69). Paraneoplastic panel and testing for demyelinating, inflammatory, and neurodegenerative disorders were negative. His weakness spontaneously resolved, but he was admitted four moths later. Repeat imaging revealed interval growth of his liver mass to 5.2x4.1cm. Liver biopsy and immunophenotypic profile (CK7+, CK20+) confirmed moderately differentiated iCCA with unusual morphologic hepatoid features (Figure 1). He succumbed to septic shock 15 days later.
Discussion: PCD presents with sudden ataxia following months of limb or trunk weakness, dysarthria, diplopia, and dysphagia. Diagnosis is challenging due to its rarity, paucity of detectable antibody responses, and need to exclude other causes. CCA has been linked to PCD due to its ability to express onconeural antigens, which can then cross-react in the brain. PCD is associated with gynecologic cancers and only two cases have been reported with CCA. iCCA displays CK7+/CK20− phenotype, while extra-hepatic CCA is CK7+/CK20+, further highlighting the unusual morphology, phenotype, and clinical presentation. This rare case underscores the need for heightened clinical vigilance for atypical manifestations of CCA to improve diagnosis and potential outcomes.
Disclosures:
Adam Khalaf, MD, Sravya Jannapureddy, MD, Harjit Singh, MD, MBA, Carl Sun, MD, Lydia Bunker, MD. P0149 - From Bile to Brain: Paraneoplastic Cerebellar Degeneration In Cholangiocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
MedStar Georgetown University Hospital, Washington, DC
Introduction: Intrahepatic cholangiocarcinoma (iCCA) is an epithelial malignancy with increasing incidence (annual percentage change 4.6%) and high mortality rates due to atypical presentations and late-stage diagnosis. Paraneoplastic syndromes in cholangiocarcinoma (CCA) are extremely rare, affect multiple organ systems, and involve dysfunctional immune responses. We present the case of a 76-year-old man with a liver lesion and neurological symptoms suggestive of acute paraneoplastic cerebellar degeneration (PCD), later diagnosed with iCCA.
Case Description/Methods: A 76-year-old male with a history of multiple myeloma, ischemic stroke, and type II diabetes presented with a 2-month history of progressive lower extremity (LE) weakness that had recently worsened, rendering him bedridden. Physical exam revealed dysarthria and diminished strength with delayed reflexes in his bilateral LE. Pan-CT imaging revealed a chronic infarct of the middle cerebral artery and an indeterminate liver lesion measuring 5.2 × 3.7 cm in segment 4 of the left hepatic lobe. One-week after admission, he developed bulbar dysphagia and tongue fasciculations. Liver enzymes were normal on arrival but peaked at AST 119 and ALT 134 nine days later. Cerebrospinal fluid (CSF) testing revealed slightly elevated glucose (80) and IgG index (0.69). Paraneoplastic panel and testing for demyelinating, inflammatory, and neurodegenerative disorders were negative. His weakness spontaneously resolved, but he was admitted four moths later. Repeat imaging revealed interval growth of his liver mass to 5.2x4.1cm. Liver biopsy and immunophenotypic profile (CK7+, CK20+) confirmed moderately differentiated iCCA with unusual morphologic hepatoid features (Figure 1). He succumbed to septic shock 15 days later.
Discussion: PCD presents with sudden ataxia following months of limb or trunk weakness, dysarthria, diplopia, and dysphagia. Diagnosis is challenging due to its rarity, paucity of detectable antibody responses, and need to exclude other causes. CCA has been linked to PCD due to its ability to express onconeural antigens, which can then cross-react in the brain. PCD is associated with gynecologic cancers and only two cases have been reported with CCA. iCCA displays CK7+/CK20− phenotype, while extra-hepatic CCA is CK7+/CK20+, further highlighting the unusual morphology, phenotype, and clinical presentation. This rare case underscores the need for heightened clinical vigilance for atypical manifestations of CCA to improve diagnosis and potential outcomes.
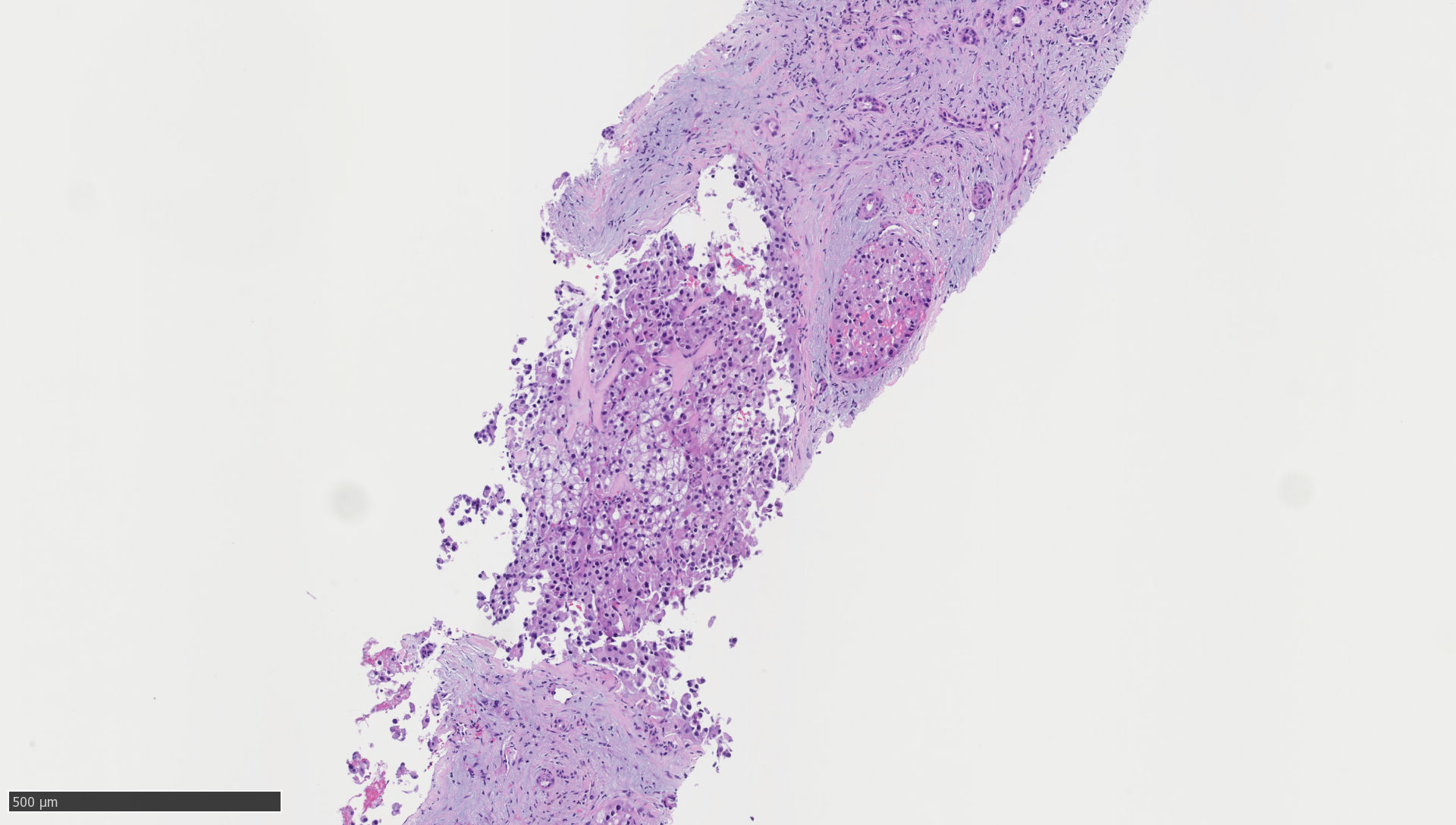
Figure: Figure 1: Histopathological analysis of intrahepatic cholangiocarcinoma. Hematoxylin-eosin staining showing nodular architecture with desmoplastic and dense myxoid/fibrous septa. Nodules showing atypical polygonal cells with pink to vesicular clear cytoplasm with some nuclei showing prominent nucleoli. No infiltrating or cribriform glands were seen.
Disclosures:
Adam Khalaf indicated no relevant financial relationships.
Sravya Jannapureddy indicated no relevant financial relationships.
Harjit Singh indicated no relevant financial relationships.
Carl Sun indicated no relevant financial relationships.
Lydia Bunker indicated no relevant financial relationships.
Adam Khalaf, MD, Sravya Jannapureddy, MD, Harjit Singh, MD, MBA, Carl Sun, MD, Lydia Bunker, MD. P0149 - From Bile to Brain: Paraneoplastic Cerebellar Degeneration In Cholangiocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

