Sunday Poster Session
Category: Biliary/Pancreas
P0150 - Diagnostic Challenges and Atypical Presentation of Cholangiocarcinoma in a Patient with Persistent Jaundice
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Ammar Hasan, MD
HCA Kingwood
Kingwood, TX
Presenting Author(s)
Ammar Hasan, MD1, Nouman Shafique, MD2, Bushra Bangash, MD3, Mahnoor Hashmi, MD1, Asad Rehman, DO1, Ismail Hader, MD1
1HCA Kingwood, Kingwood, TX; 2AdventHealth Medical Group, AdventHealth, Orlando, FL; 3HCA Kingwood, Houston, TX
Introduction: Cholangiocarcinoma, an aggressive bile duct malignancy, presents diagnostic challenges due to its variable symptoms and overlap with other hepatobiliary diseases. This case highlights the importance of comprehensive evaluation in patients with persistent jaundice despite initial non-diagnostic imaging.
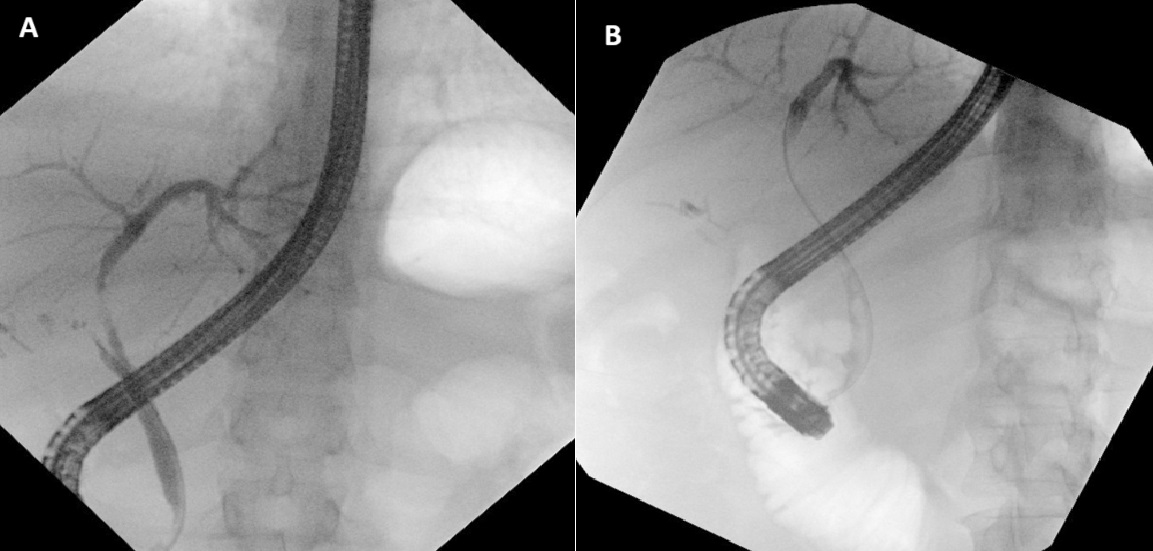
Case Description/Methods: A 54-year-old female with a past medical history of Crohn's disease and recent cholecystectomy presented with two weeks of pruritus, pale stools, jaundice, dark urine, and intermittent nausea. Initial labs showed elevated liver function tests (Total Bilirubin 4.2, AST 224, ALT 319, and Alkaline Phosphatase 959). CT scan at an outside ER indicated possible ductal dilation and possible liver abscess which prompted her to be admitted to the hospital. At our facility, an Ultrasound and CT abdomen/pelvis showed no biliary dilation or liver abscess. Persistent symptoms and uptrending liver function tests led to a further work-up including MRCP, which was negative for ductal dilation. Autoimmune workup and cancer biomarkers were negative. Liver biopsy results were non-specific. An ERCP identified a retained common bile duct (CBD) stone and biliary strictures (Figures A and B), managed with stent placement. The patient’s symptoms temporarily improved, but LFTs remained elevated. In three months, She was readmitted twice with recurrent jaundice and elevated LFTs. Repeat ERCP was done during her second hospitalization which showed another stricture and the first set of biopsies taken from the common bile duct came back inconclusive. During her third hospitalization, a repeat ERCP was done again during which another set of biopsies was taken from the common bile duct which confirmed Cholangiocarcinoma. The patient was then scheduled for chemotherapy and potential surgery.
Discussion: This case highlights the challenges in diagnosing cholangiocarcinoma, especially with initial non-diagnostic imaging and overlapping autoimmune features. Persistent jaundice and elevated LFTs necessitated repeated and advanced diagnostic procedures, including ERCP and biopsy. Considering this patient’s history of Crohn's disease, our initial working diagnoses were Primary biliary cirrhosis (PBC) and Primary sclerosing cholangitis (PSC). The difficulty of non-diagnostic initial imaging complicates timely identification and management. Clinicians should consider cholangiocarcinoma in similar cases with persistent symptoms to ensure timely diagnosis and treatment, despite initial imaging challenges.
Disclosures:
Ammar Hasan, MD1, Nouman Shafique, MD2, Bushra Bangash, MD3, Mahnoor Hashmi, MD1, Asad Rehman, DO1, Ismail Hader, MD1. P0150 - Diagnostic Challenges and Atypical Presentation of Cholangiocarcinoma in a Patient with Persistent Jaundice, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1HCA Kingwood, Kingwood, TX; 2AdventHealth Medical Group, AdventHealth, Orlando, FL; 3HCA Kingwood, Houston, TX
Introduction: Cholangiocarcinoma, an aggressive bile duct malignancy, presents diagnostic challenges due to its variable symptoms and overlap with other hepatobiliary diseases. This case highlights the importance of comprehensive evaluation in patients with persistent jaundice despite initial non-diagnostic imaging.
Case Description/Methods: A 54-year-old female with a past medical history of Crohn's disease and recent cholecystectomy presented with two weeks of pruritus, pale stools, jaundice, dark urine, and intermittent nausea. Initial labs showed elevated liver function tests (Total Bilirubin 4.2, AST 224, ALT 319, and Alkaline Phosphatase 959). CT scan at an outside ER indicated possible ductal dilation and possible liver abscess which prompted her to be admitted to the hospital. At our facility, an Ultrasound and CT abdomen/pelvis showed no biliary dilation or liver abscess. Persistent symptoms and uptrending liver function tests led to a further work-up including MRCP, which was negative for ductal dilation. Autoimmune workup and cancer biomarkers were negative. Liver biopsy results were non-specific. An ERCP identified a retained common bile duct (CBD) stone and biliary strictures (Figures A and B), managed with stent placement. The patient’s symptoms temporarily improved, but LFTs remained elevated. In three months, She was readmitted twice with recurrent jaundice and elevated LFTs. Repeat ERCP was done during her second hospitalization which showed another stricture and the first set of biopsies taken from the common bile duct came back inconclusive. During her third hospitalization, a repeat ERCP was done again during which another set of biopsies was taken from the common bile duct which confirmed Cholangiocarcinoma. The patient was then scheduled for chemotherapy and potential surgery.
Discussion: This case highlights the challenges in diagnosing cholangiocarcinoma, especially with initial non-diagnostic imaging and overlapping autoimmune features. Persistent jaundice and elevated LFTs necessitated repeated and advanced diagnostic procedures, including ERCP and biopsy. Considering this patient’s history of Crohn's disease, our initial working diagnoses were Primary biliary cirrhosis (PBC) and Primary sclerosing cholangitis (PSC). The difficulty of non-diagnostic initial imaging complicates timely identification and management. Clinicians should consider cholangiocarcinoma in similar cases with persistent symptoms to ensure timely diagnosis and treatment, despite initial imaging challenges.
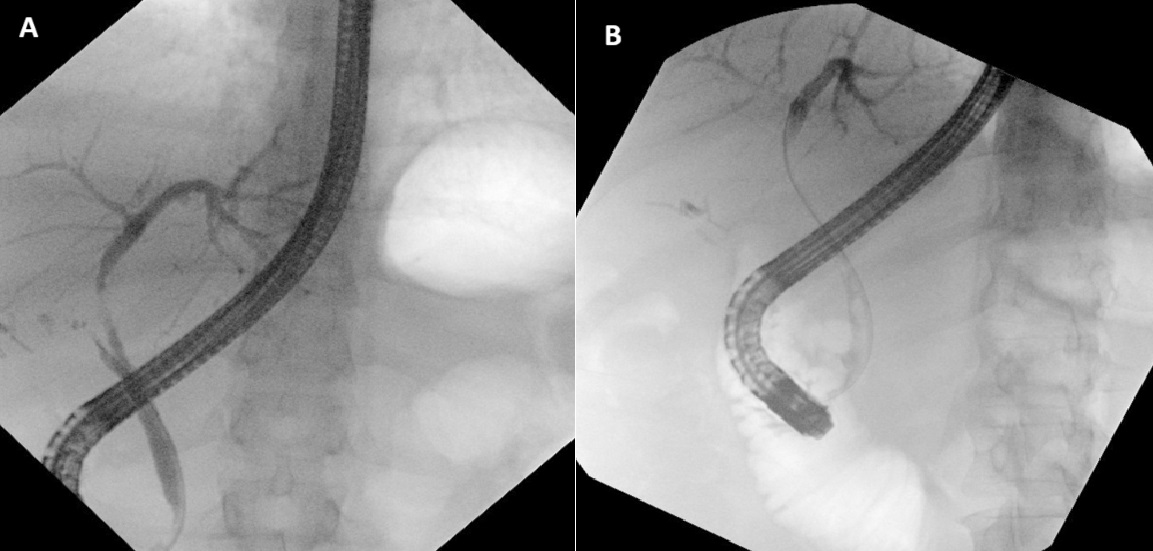
Figure: ERCP showing common bile duct strictures
Disclosures:
Ammar Hasan indicated no relevant financial relationships.
Nouman Shafique indicated no relevant financial relationships.
Bushra Bangash indicated no relevant financial relationships.
Mahnoor Hashmi indicated no relevant financial relationships.
Asad Rehman indicated no relevant financial relationships.
Ismail Hader indicated no relevant financial relationships.
Ammar Hasan, MD1, Nouman Shafique, MD2, Bushra Bangash, MD3, Mahnoor Hashmi, MD1, Asad Rehman, DO1, Ismail Hader, MD1. P0150 - Diagnostic Challenges and Atypical Presentation of Cholangiocarcinoma in a Patient with Persistent Jaundice, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
