Sunday Poster Session
Category: Biliary/Pancreas
P0151 - Pyogenic Hepatic Abscesses Secondary to Ascending Cholangitis 13 Years Post-Cholecystectomy: A Case Report
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Milaris Sanchez-Cordero, MD
Mayaguez Medical Center
Mayaguez, PR
Presenting Author(s)
Milaris Sanchez-Cordero, MD1, Yue-Sai Jao-Ayala, MD2, Francisco Cebollero-Santamaria, MD1, Karla Velez-Rivera, MD1, Milton Carrero-Quinones, MD1, Marcos Chacon, MD1
1Mayaguez Medical Center, Mayaguez, Puerto Rico; 2University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico
Introduction: Cholecystectomy is the definitive treatment of acute cholecystitis. Post-cholecystectomy syndrome occurs after surgery and presents with the persistence of biliary colic with gastrointestinal symptoms similar to those in patients with cholecystitis prior to surgery. Post-cholecystectomy choledocholithiasis is a rare complication after cholecystectomy with an incidence of 0.4 %. An uncommon complication of choledocholithiasis is the development of pyogenic hepatic abscesses that commonly involve polymicrobial infection, usually with E. coli and Klebsiella. If left untreated, these abscesses can progress to peritonitis or sepsis, but when treated, the mortality decreases to 10-30%. There is a lack of data on the incidence of post-cholecystectomy choledocholithiasis leading to hepatic abscesses. It is estimated that there are 2–15 cases of hepatic abscesses per 100,000 people in the US and half of these are caused by cholangitis.
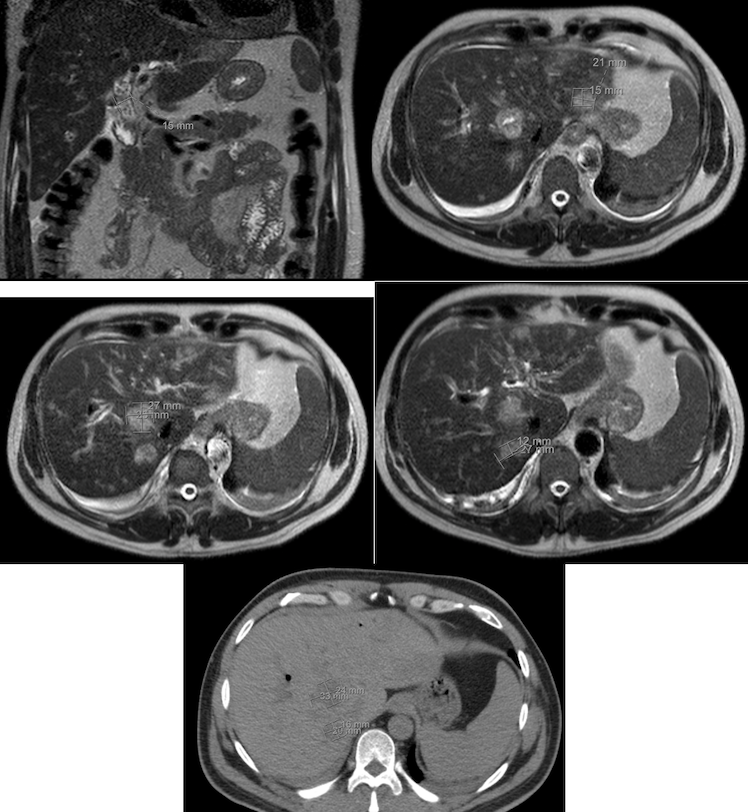
Case Description/Methods: This is a case of a 51-year-old male patient with a history of HIV and recurrent episodes of cholangitis post cholecystectomy who presented to the Emergency Department complaining of severe abdominal pain for one week of evolution. The patient reported pain as constant and non-radiating. The patient presented with sepsis criteria with suspected ascending cholangitis as a foci. The patient was admitted and treated with empiric antibiotic therapy. Abdomen CT showed intrahepatic biliary ductal dilation with pneumobilia. MRCP showed multiple hepatic lesions compatible with developing abscesses. The patient underwent ERCP, which showed no choledocolithiasis with the presence of hepatic abscesses without communication with the bile ducts. Abscess culture results positive for Klebsiella and E.Coli with percutaneous drainage of the most considerable abscess. Antibiotic therapy was given for six weeks and repeated Abdomen CT demonstrate a nearly complete resolution of the abscess.
Discussion: Given the infrequency of cholangitis-induced pyogenic hepatic abscesses, as well as the low incidence of choledocholithiasis in post-cholecystectomy patients, pyogenic hepatic abscesses secondary to post-cholecystectomy choledocholithiasis comprise a rare entity. This case showed us the importance of contemplating this type of complication in patients with recurrent episodes of cholangitis despite not having the classic presentation. Early treatment with antimicrobial therapy, surgery, and multidisciplinary team intervention are critical and can avoid fatal outcomes.
Disclosures:
Milaris Sanchez-Cordero, MD1, Yue-Sai Jao-Ayala, MD2, Francisco Cebollero-Santamaria, MD1, Karla Velez-Rivera, MD1, Milton Carrero-Quinones, MD1, Marcos Chacon, MD1. P0151 - Pyogenic Hepatic Abscesses Secondary to Ascending Cholangitis 13 Years Post-Cholecystectomy: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayaguez Medical Center, Mayaguez, Puerto Rico; 2University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico
Introduction: Cholecystectomy is the definitive treatment of acute cholecystitis. Post-cholecystectomy syndrome occurs after surgery and presents with the persistence of biliary colic with gastrointestinal symptoms similar to those in patients with cholecystitis prior to surgery. Post-cholecystectomy choledocholithiasis is a rare complication after cholecystectomy with an incidence of 0.4 %. An uncommon complication of choledocholithiasis is the development of pyogenic hepatic abscesses that commonly involve polymicrobial infection, usually with E. coli and Klebsiella. If left untreated, these abscesses can progress to peritonitis or sepsis, but when treated, the mortality decreases to 10-30%. There is a lack of data on the incidence of post-cholecystectomy choledocholithiasis leading to hepatic abscesses. It is estimated that there are 2–15 cases of hepatic abscesses per 100,000 people in the US and half of these are caused by cholangitis.
Case Description/Methods: This is a case of a 51-year-old male patient with a history of HIV and recurrent episodes of cholangitis post cholecystectomy who presented to the Emergency Department complaining of severe abdominal pain for one week of evolution. The patient reported pain as constant and non-radiating. The patient presented with sepsis criteria with suspected ascending cholangitis as a foci. The patient was admitted and treated with empiric antibiotic therapy. Abdomen CT showed intrahepatic biliary ductal dilation with pneumobilia. MRCP showed multiple hepatic lesions compatible with developing abscesses. The patient underwent ERCP, which showed no choledocolithiasis with the presence of hepatic abscesses without communication with the bile ducts. Abscess culture results positive for Klebsiella and E.Coli with percutaneous drainage of the most considerable abscess. Antibiotic therapy was given for six weeks and repeated Abdomen CT demonstrate a nearly complete resolution of the abscess.
Discussion: Given the infrequency of cholangitis-induced pyogenic hepatic abscesses, as well as the low incidence of choledocholithiasis in post-cholecystectomy patients, pyogenic hepatic abscesses secondary to post-cholecystectomy choledocholithiasis comprise a rare entity. This case showed us the importance of contemplating this type of complication in patients with recurrent episodes of cholangitis despite not having the classic presentation. Early treatment with antimicrobial therapy, surgery, and multidisciplinary team intervention are critical and can avoid fatal outcomes.
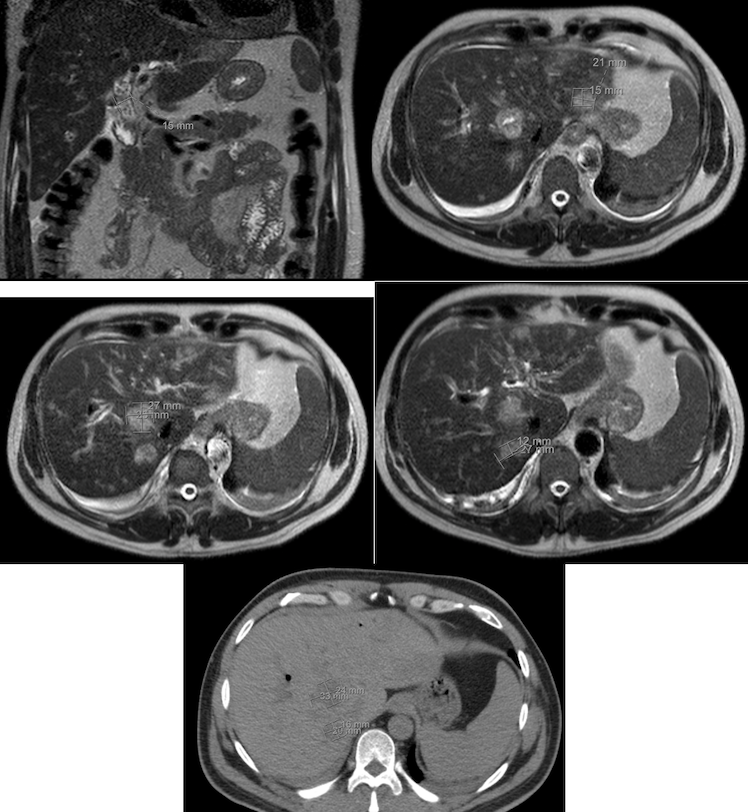
Figure: Liver Abscesses in MRCP and Abdomen CT
Disclosures:
Milaris Sanchez-Cordero indicated no relevant financial relationships.
Yue-Sai Jao-Ayala indicated no relevant financial relationships.
Francisco Cebollero-Santamaria indicated no relevant financial relationships.
Karla Velez-Rivera indicated no relevant financial relationships.
Milton Carrero-Quinones indicated no relevant financial relationships.
Marcos Chacon indicated no relevant financial relationships.
Milaris Sanchez-Cordero, MD1, Yue-Sai Jao-Ayala, MD2, Francisco Cebollero-Santamaria, MD1, Karla Velez-Rivera, MD1, Milton Carrero-Quinones, MD1, Marcos Chacon, MD1. P0151 - Pyogenic Hepatic Abscesses Secondary to Ascending Cholangitis 13 Years Post-Cholecystectomy: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
