Sunday Poster Session
Category: Biliary/Pancreas
P0159 - Pancreaticopleural Fistula and Pseudocyst Formation with Bilateral Pleural Effusions Secondary to Pancreatic Adenocarcinoma
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Vivek V. Jasti, MD
OhioHealth Riverside Methodist Hospital
Columbus, OH
Presenting Author(s)
Vivek V. Jasti, MD1, Tannaz Rowshanbakhtfardian, MD2, Kim Jordan, MD3, David Y. Lo, MD4
1OhioHealth Riverside Methodist Hospital, Columbus, OH; 2OhioHealth, Columbus, OH; 3OhioHealth Riverside Methodist Hospital, Powell, OH; 4Ohio Gastroenterology Group, New Albany, OH
Introduction: Pancreaticopleural fistula (PPF) is a rare cause of pleural effusion and very rarely associated with malignancy. We present a case of PPF and pseudocyst formation as the initial presenting symptom of pancreatic adenocarcinoma.
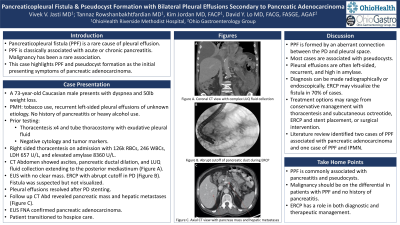
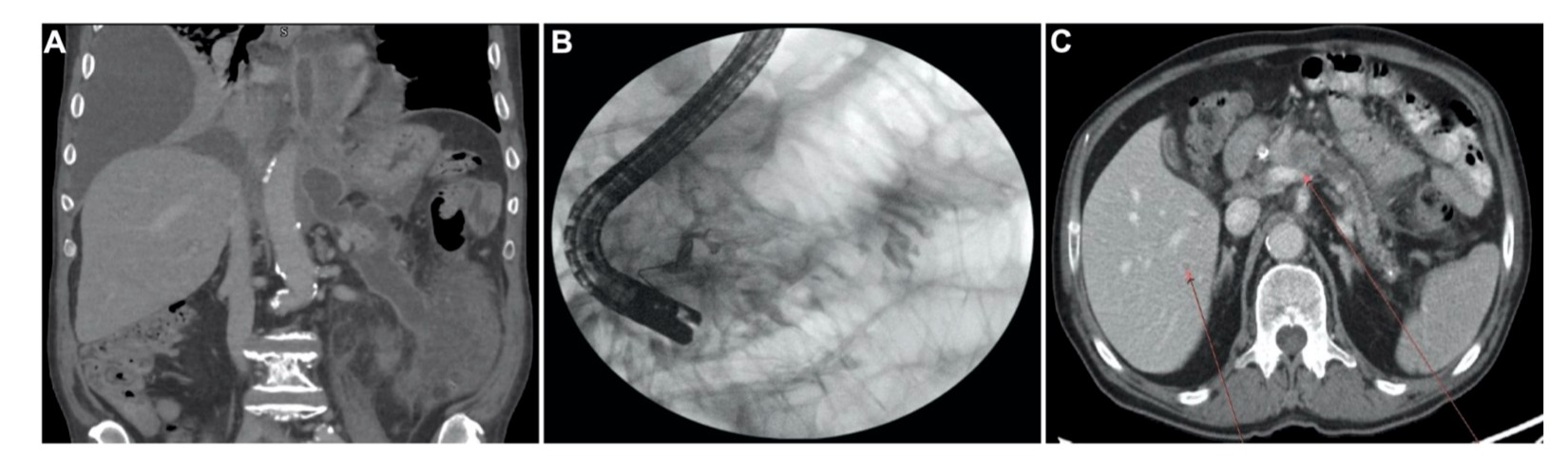
Case Description/Methods: 73-year-old male with history of tobacco use and recurrent left-sided pleural effusions presented with dyspnea and a new, large right-sided pleural effusion. For the last 4 months, he had 50 lb. weight loss and left-sided pleural effusions of unknown etiology. He had no history of pancreatitis or heavy alcohol use. He underwent 4 thoracenteses and tube thoracostomy. Prior pleural fluid analyses were exudative; cytology and tumor markers were negative. Right-sided thoracentesis revealed 126k RBCs, 246 WBCs, LDH 657 U/L, and elevated amylase of 8360 U/L. CT showed ascites, pancreatic ductal (PD) dilation, and a fluid collection from the left upper quadrant to the posterior mediastinum (Figure A). EUS and ERCP performed for suspected PD disruption revealed an atrophic pancreas with abrupt cutoff of the PD in the body but no clear mass (Figure B). A fistula was not visualized but suspected. PD stenting resulted in temporary resolution of pleural effusions. Follow up CT 9 months later revealed a pancreatic mass and hepatic metastases (Figure C). EUS fine needle aspiration confirmed pancreatic adenocarcinoma. The patient was started on gemcitabine but shortly afterwards elected for hospice.
Discussion: PPF is formed by an aberrant connection between the PD and pleural space. Pseudocysts are present in about 70% of cases as drainage commonly occurs due to a premature or ruptured pseudocyst. Pleural effusion is often recurrent, left-sided, and high in amylase. PPF is classically associated with acute/chronic pancreatitis. It has rarely been associated with pancreatic malignancy. Literature review found two prior cases of PPF associated with pancreatic adenocarcinoma, and one case associated with intraductal papillary mucinous neoplasm. Diagnosis of PPF can be made radiographically demonstrating a fistulous tract, or endoscopically with ERCP. ERCP is diagnostic in 80% and visualizes the fistula in 70% of cases. Treatment options for PPF include conservative management with drainage of pleural fluid and subcutaneous octreotide, ERCP and PD stent placement, or surgery. A high index of suspicion for malignancy should be present in PPF without obvious risk factors for chronic pancreatitis.
Disclosures:
Vivek V. Jasti, MD1, Tannaz Rowshanbakhtfardian, MD2, Kim Jordan, MD3, David Y. Lo, MD4. P0159 - Pancreaticopleural Fistula and Pseudocyst Formation with Bilateral Pleural Effusions Secondary to Pancreatic Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1OhioHealth Riverside Methodist Hospital, Columbus, OH; 2OhioHealth, Columbus, OH; 3OhioHealth Riverside Methodist Hospital, Powell, OH; 4Ohio Gastroenterology Group, New Albany, OH
Introduction: Pancreaticopleural fistula (PPF) is a rare cause of pleural effusion and very rarely associated with malignancy. We present a case of PPF and pseudocyst formation as the initial presenting symptom of pancreatic adenocarcinoma.
Case Description/Methods: 73-year-old male with history of tobacco use and recurrent left-sided pleural effusions presented with dyspnea and a new, large right-sided pleural effusion. For the last 4 months, he had 50 lb. weight loss and left-sided pleural effusions of unknown etiology. He had no history of pancreatitis or heavy alcohol use. He underwent 4 thoracenteses and tube thoracostomy. Prior pleural fluid analyses were exudative; cytology and tumor markers were negative. Right-sided thoracentesis revealed 126k RBCs, 246 WBCs, LDH 657 U/L, and elevated amylase of 8360 U/L. CT showed ascites, pancreatic ductal (PD) dilation, and a fluid collection from the left upper quadrant to the posterior mediastinum (Figure A). EUS and ERCP performed for suspected PD disruption revealed an atrophic pancreas with abrupt cutoff of the PD in the body but no clear mass (Figure B). A fistula was not visualized but suspected. PD stenting resulted in temporary resolution of pleural effusions. Follow up CT 9 months later revealed a pancreatic mass and hepatic metastases (Figure C). EUS fine needle aspiration confirmed pancreatic adenocarcinoma. The patient was started on gemcitabine but shortly afterwards elected for hospice.
Discussion: PPF is formed by an aberrant connection between the PD and pleural space. Pseudocysts are present in about 70% of cases as drainage commonly occurs due to a premature or ruptured pseudocyst. Pleural effusion is often recurrent, left-sided, and high in amylase. PPF is classically associated with acute/chronic pancreatitis. It has rarely been associated with pancreatic malignancy. Literature review found two prior cases of PPF associated with pancreatic adenocarcinoma, and one case associated with intraductal papillary mucinous neoplasm. Diagnosis of PPF can be made radiographically demonstrating a fistulous tract, or endoscopically with ERCP. ERCP is diagnostic in 80% and visualizes the fistula in 70% of cases. Treatment options for PPF include conservative management with drainage of pleural fluid and subcutaneous octreotide, ERCP and PD stent placement, or surgery. A high index of suspicion for malignancy should be present in PPF without obvious risk factors for chronic pancreatitis.
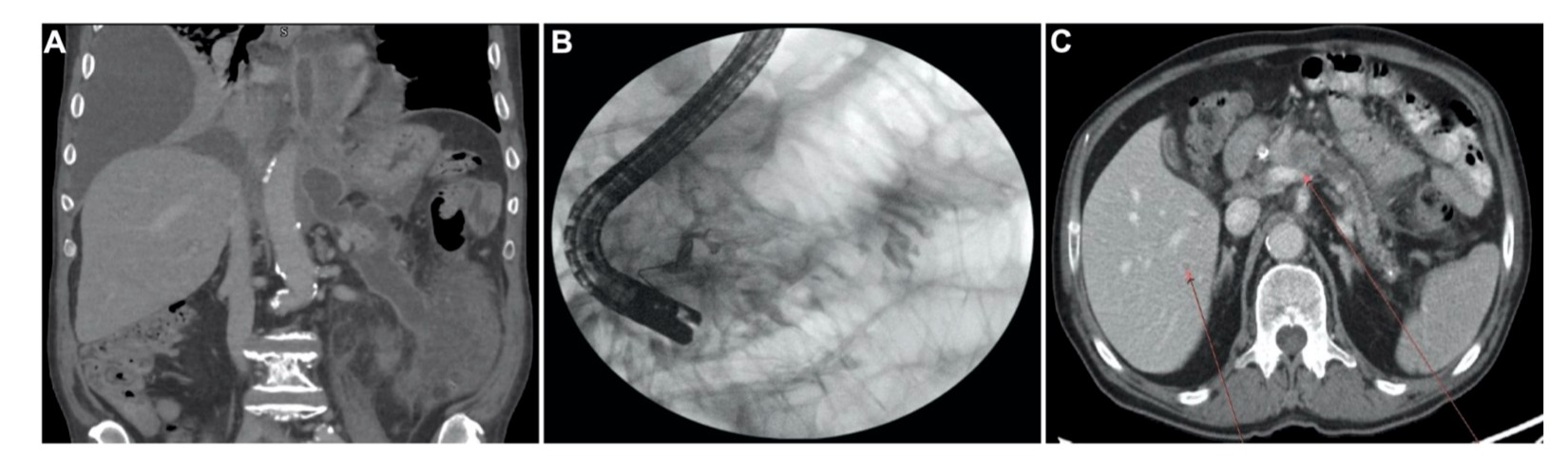
Figure: Figure A) Coronal view CT with peripancreatic fluid collection with extension to the posterior mediastinum
Figure B) ERCP with filling defect on pancreatogram
Figure C) Follow up axial view CT with pancreatic mass and hepatic metastases
Figure B) ERCP with filling defect on pancreatogram
Figure C) Follow up axial view CT with pancreatic mass and hepatic metastases
Disclosures:
Vivek Jasti indicated no relevant financial relationships.
Tannaz Rowshanbakhtfardian indicated no relevant financial relationships.
Kim Jordan indicated no relevant financial relationships.
David Lo: Abbvie – Speakers Bureau. QOL – Speakers Bureau.
Vivek V. Jasti, MD1, Tannaz Rowshanbakhtfardian, MD2, Kim Jordan, MD3, David Y. Lo, MD4. P0159 - Pancreaticopleural Fistula and Pseudocyst Formation with Bilateral Pleural Effusions Secondary to Pancreatic Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
