Sunday Poster Session
Category: Biliary/Pancreas
P0161 - A Rare Convergence: Pancreatic Cancer Arising in the Setting of Autoimmune Pancreatitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Abdelrahman Yakout, MD
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Abdelrahman Yakout, MD, Daniela Fluxa, MD, Aziza Nassar, MD, MPH, Victoria Gómez, MD
Mayo Clinic, Jacksonville, FL
Introduction: Autoimmune pancreatitis (AIP) is a rare fibroinflammatory, autoimmune chronic pancreatic disease which often responds to treatment with corticosteroids. Although chronic pancreatitis is a risk factor for pancreatic cancer, AIP association with pancreatic cancer has been controversial. We report a case of a patient with Type 1 AIP who developed pancreatic cancer.
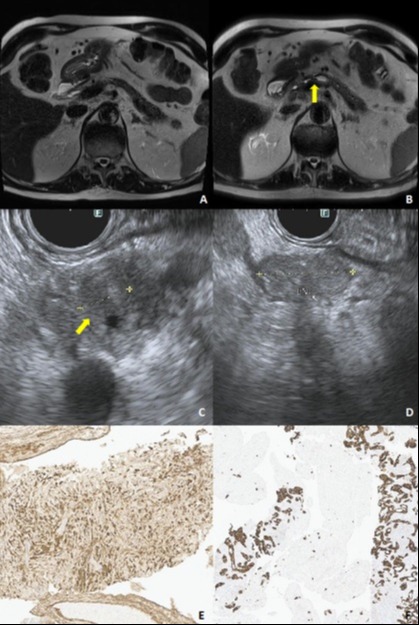
Case Description/Methods: A 76-year-old man with history of type 2 diabetes presented with abdominal pain in 2020. Work-up revealed elevated lipase and amylase levels and was diagnosed with acute pancreatitis. Months later, he presented with obstructive jaundice. Magnetic resonance cholangiopancreatography (MRCP) revealed a mass in the pancreas head/body and a distal common bile duct stricture. Endoscopic ultrasound (EUS) with fine needle biopsy (EUS-FNB) was performed along with endoscopic retrograde cholangiopancreatography (ERCP) with placement of a biliary stent. Histopathology revealed lymphoplasmacytic infiltration and increased number of IgG4-positive plasma cells (up to 34/hpf). A diagnosis of type 1 AIP was confirmed, and prednisone was started with remarkable improvement in symptoms, resolution of jaundice, and imaging. The stent was subsequently removed, with resolution of the biliary stricture. Prednisone was slowly tapered over a course of 1.5 years due to difficulty with controlling blood glucose levels. Surveillance imaging with MRCP continued to ensure resolution of the biliary stricture. During follow up, 3 years after being diagnosed with AIP, follow up MRCP showed dilation of the main pancreatic duct (PD) with prominent narrowing at the neck/body junction (Figure 1). EUS showed a dilated PD at the neck/body junction and three enlarged porta hepatis lymph nodes (Figure 1). No obvious mass was seen but given the abrupt change in PD caliber, EUS/FNB was performed in this area. Histopathology revealed atypical mucinous epithelium suggestive of intraductal papillary mucinous neoplasm arising on a background of sclerosing pancreatitis confirmed with a positive IgG4 positive plasma cell parenchymal infiltrate ( >20/hpf). Lymph node FNB showed metastatic pancreatic adenocarcinoma (Figure 1). The patient was started on neoadjuvant chemotherapy.
Discussion: Pancreatic cancer arising in a background of AIP is rare, and the correlation between the two illnesses is unclear. Patients with AIP who are clinically in remission should be followed closely. Changes in PD caliber should raise concern and prompt further investigations.
Disclosures:
Abdelrahman Yakout, MD, Daniela Fluxa, MD, Aziza Nassar, MD, MPH, Victoria Gómez, MD. P0161 - A Rare Convergence: Pancreatic Cancer Arising in the Setting of Autoimmune Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic, Jacksonville, FL
Introduction: Autoimmune pancreatitis (AIP) is a rare fibroinflammatory, autoimmune chronic pancreatic disease which often responds to treatment with corticosteroids. Although chronic pancreatitis is a risk factor for pancreatic cancer, AIP association with pancreatic cancer has been controversial. We report a case of a patient with Type 1 AIP who developed pancreatic cancer.
Case Description/Methods: A 76-year-old man with history of type 2 diabetes presented with abdominal pain in 2020. Work-up revealed elevated lipase and amylase levels and was diagnosed with acute pancreatitis. Months later, he presented with obstructive jaundice. Magnetic resonance cholangiopancreatography (MRCP) revealed a mass in the pancreas head/body and a distal common bile duct stricture. Endoscopic ultrasound (EUS) with fine needle biopsy (EUS-FNB) was performed along with endoscopic retrograde cholangiopancreatography (ERCP) with placement of a biliary stent. Histopathology revealed lymphoplasmacytic infiltration and increased number of IgG4-positive plasma cells (up to 34/hpf). A diagnosis of type 1 AIP was confirmed, and prednisone was started with remarkable improvement in symptoms, resolution of jaundice, and imaging. The stent was subsequently removed, with resolution of the biliary stricture. Prednisone was slowly tapered over a course of 1.5 years due to difficulty with controlling blood glucose levels. Surveillance imaging with MRCP continued to ensure resolution of the biliary stricture. During follow up, 3 years after being diagnosed with AIP, follow up MRCP showed dilation of the main pancreatic duct (PD) with prominent narrowing at the neck/body junction (Figure 1). EUS showed a dilated PD at the neck/body junction and three enlarged porta hepatis lymph nodes (Figure 1). No obvious mass was seen but given the abrupt change in PD caliber, EUS/FNB was performed in this area. Histopathology revealed atypical mucinous epithelium suggestive of intraductal papillary mucinous neoplasm arising on a background of sclerosing pancreatitis confirmed with a positive IgG4 positive plasma cell parenchymal infiltrate ( >20/hpf). Lymph node FNB showed metastatic pancreatic adenocarcinoma (Figure 1). The patient was started on neoadjuvant chemotherapy.
Discussion: Pancreatic cancer arising in a background of AIP is rare, and the correlation between the two illnesses is unclear. Patients with AIP who are clinically in remission should be followed closely. Changes in PD caliber should raise concern and prompt further investigations.
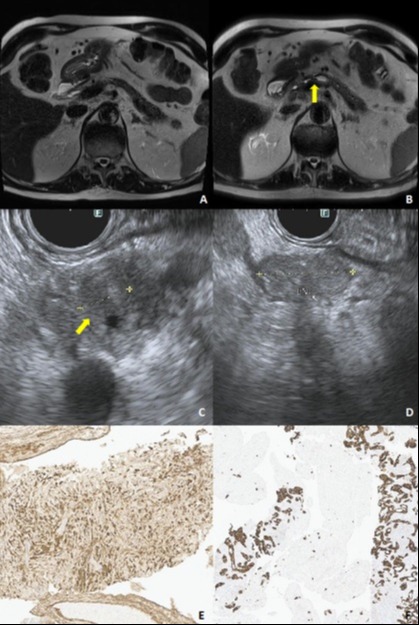
Figure: A. MRI 10/2022 showing stable chronic autoimmune pancreatitis with pancreatic atrophy and multiple dilated pancreatic ducts side branches.
B. MRI 1/2024 showing focal stricture in the pancreatic neck without clear obstructing mass (yellow arrow).
C. Area of PD transition point in the body/neck of the pancreas where FNB was performed (yellow arrow).
D. Lymph node seen in the porta hepatis on EUS.
E. Pancreas core biopsies showing IgG4 related sclerosing pancreatitis with extensive lymphoplasmatic infiltrate with positive IgG4 plasma cells immunostain.
F. Lymph node core biopsies with positive CK7 immunoreactivity showing metastatic adenocarcinoma consistent with pancreatic primary.
B. MRI 1/2024 showing focal stricture in the pancreatic neck without clear obstructing mass (yellow arrow).
C. Area of PD transition point in the body/neck of the pancreas where FNB was performed (yellow arrow).
D. Lymph node seen in the porta hepatis on EUS.
E. Pancreas core biopsies showing IgG4 related sclerosing pancreatitis with extensive lymphoplasmatic infiltrate with positive IgG4 plasma cells immunostain.
F. Lymph node core biopsies with positive CK7 immunoreactivity showing metastatic adenocarcinoma consistent with pancreatic primary.
Disclosures:
Abdelrahman Yakout indicated no relevant financial relationships.
Daniela Fluxa indicated no relevant financial relationships.
Aziza Nassar indicated no relevant financial relationships.
Victoria Gómez: COOKMedical – Education and Lectures. Olympus – Consultant.
Abdelrahman Yakout, MD, Daniela Fluxa, MD, Aziza Nassar, MD, MPH, Victoria Gómez, MD. P0161 - A Rare Convergence: Pancreatic Cancer Arising in the Setting of Autoimmune Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

